Why Might Schizophrenia Be More Severe in Men?
A number of studies have found that when it comes to having schizophrenia, being female is a plus. Now a 20-year longitudinal study—purportedly the longest ever of the subject—has found the same thing. In essence, women with schizophrenia experience less intense levels of psychosis, better global functioning, and greater recovery than men with schizophrenia do.
The study was headed by Linda Grossman, Ph.D., of the University of Illinois at Chicago. Results were posted on the Schizophrenia Research Web site on June 3 and are now in press.
The study included 54 men and 43 women with schizophrenia or other psychotic disorders. All were first evaluated while hospitalized because of psychosis and then evaluated six more times over the following 20 years regarding the presence of psychosis, global outcome, and rate of recovery. (Recovery was defined as the absence of major symptoms, no rehospitalizations, and partly adequate work and social functioning for at least a year.)
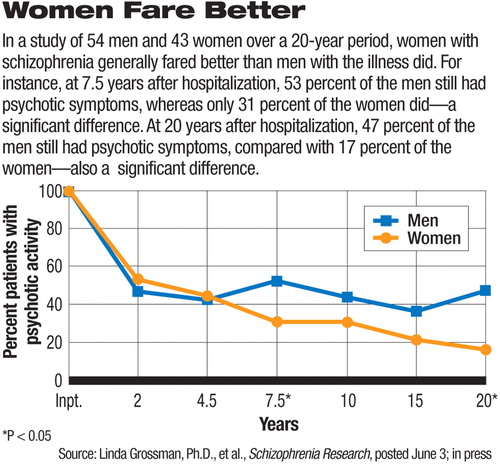
The women, but not the men, showed a significant lessening of psychosis over the 20-year period. The women showed significantly better global functioning than the men did during three of the six follow-up periods. And 61 percent of the women recovered at some point during the 20-year period, while only 41 percent of the men did.
But why? Is it because women tend to get schizophrenia later in life, and this extra reprieve gives them time to develop more knowledge, social skills, and worldly experience that they can then deploy when schizophrenia strikes? This is one possibility suggested by the investigators, but probably not for the women in this particular cohort since they already had schizophrenia in their early 20s, just as the men did.
Another possibility is that women are better shielded from schizophrenia because they have more of the hormone estrogen in their bodies. Indeed, there is some evidence that female schizophrenia patients' psychosis waxes and wanes with their menstrual cycles—that is, peaks when estrogen is low in their bodies and ebbs when estrogen is high.
Another study, published in the August Archives of General Psychiatry, bolsters the case that estrogen is a natural antipsychotic agent.
Jayashri Kulkarni, Ph.D., director of the Psychiatry Research Center at the Alfred and Monash University in Melbourne, Australia, and her colleagues randomized 102 premenopausal women with schizophrenia to receive either an estrogen skin patch or a placebo skin patch for 28 days. All of the women remained on their antipsychotic medication regimens during this period. There were no significant differences between the estrogen and placebo groups in age, age at illness onset, or antipsychotic medication dosage. The women receiving estrogen experienced significantly fewer positive symptoms (although not significantly fewer negative symptoms) during the study period.
“Estrogen treatment is a promising new area for future treatment of schizophrenia,” Kulkarni and her group concluded.
And as Kulkarni told Psychiatric News, she and her colleagues are now attempting to replicate their findings in a three-site study of 180 premenopausal women with schizophrenia. They have also completed a double-blind, placebo-controlled, two-week trial to see whether estrogen supplements can help men with schizophrenia.
Their data suggest that it can. The challenge of giving men estrogen over the long term, of course, is the danger of feminization, Kulkarni acknowledged. Nonetheless, she stressed, the results indicate that estrogen has“ the same potential brain effects, that is, through dopamine and serotonin, in men as in women.”
The study conducted by Grossman and colleagues was partly funded by the U.S. Public Health Service and the National Institute of Mental Health. The study by Kulkarni and colleagues was funded by the Stanley Medical Research Institute, National Health and Medical Research Council of Australia, and NARSAD: the Mental Health Research Association.
An abstract of “Sex Differences in Schizophrenia and Other Psychotic Disorders: A 20-Year Longitudinal Study of Psychosis and Recovery” can be accessed at<www.sciencedirect.com> by clicking “Browse by Title,” then “S,” and then“ Schizophrenia Research.” An abstract of “Estrogen in Severe Mental Illness” is posted at<http://archpsyc.ama-assn.org/cgi/content/short/65/8/955>.▪



