CDC Finds Most With Depression Fail to Seek Specialized Care
More than 1 in 20 Americans older than age 11 may have depression, according to an analysis from the Centers for Disease Prevention and Control (CDC). That's about 5 percent of individuals in this age group.
Researcher Laura Pratt, Ph.D., of the Office of Analysis and Epidemiology at the CDC's National Center for Health Statistics, and CDC colleague Deborah Brody, M.P.H., based their finding on a data analysis of the National Health and Nutrition Examination Survey (NHANES) from 2005-2006. The NHANES used a nine-item screening tool to ask those surveyed in face-to-face interviews about “depressive symptoms” they had experienced during the prior two weeks. The analysis was released in September.
The researchers found depression rates were higher in people aged 40 to 59, women, and non-Hispanic black people than in other demographic groups. Rates of depression were higher among low-income individuals than among those with higher incomes.
“Depression is a major public health problem, and increasing the number of Americans with depression who receive treatment is an important public health goal and a national objective of Healthy People 2010,” wrote Pratt and Brody, referring to the federal health goals for the nation. Brody works in the CDC's Division of Health and Nutrition Examination Surveys.
NHANES is a continuous cross-sectional survey of the civilian, noninstitutionalized U.S. population designed to assess the health and nutrition of Americans. The survey participants completed a face-to-face“ household interview” and had an examination in a mobile examination center that included a private interview. More than 5,000 people were included in the 2005 to 2006 NHANES, which also oversampled blacks and Mexican Americans, adults over age 60, and individuals of low income in order to “improve the statistical reliability of the estimates for these groups,” according to the researchers.
The depression rates found in the CDC analysis are lower than those found in some previous research. For example, major depression was estimated to affect about 9 percent of adolescents aged 12 through 17 and 7.6 percent of adults over the preceding year in data released by the Substance Abuse and Mental Health Services Administration in June 2007 (Psychiatric News, August 3, 2007).
The CDC report also found that 80 percent of people who reported symptoms of depression also reported some degree of “functional impairment” due to their depression; and 27 percent reported “serious difficulties” in work and home life. About 35 percent of male respondents and 22 percent of female respondents with depression symptoms reported that their symptoms made it “very or extremely difficult” for them to work, get things done at home, or get along with other people. More than half of the people with mild depressive symptoms also reported some difficulty in daily functioning attributable to their symptoms.
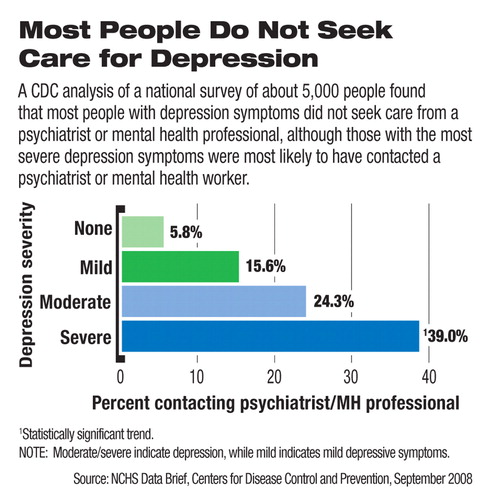
Among the most startling findings for psychiatrists and mental health professionals was that only 29 percent of respondents with depression symptoms reported contacting a mental health clinician in the prior year. In a subset of respondents with severe depression scores, only 39 percent made contact with a psychiatrist, psychologist, psychiatric nurse, or clinical social worker.
“There are many reasons people with depression do not receive treatment,” said Pratt and Brody. “Some do not realize they have an illness that can be treated. Others do not believe treatment works. Other barriers to treatment include the stigma surrounding mental illness and mental health treatment and lack of insurance coverage for mental health care.”
The survey's findings of “contact” rates may not reflect actual treatment rates, because the respondents who contacted a psychiatrist or mental health professional were not asked if they actually began treatment for depression. Also, the survey did not ask about mental health treatment received from primary care providers.
The survey's findings on rates of depression generally reflect those of previous research, Laurence Miller, M.D., chair of APA's Committee on Public Funding for Psychiatric Services, told Psychiatric News.
The finding that few with mental illness seek care from psychiatrists and mental health professionals probably reflects the common dependence of most Americans on general practice physicians for their health care. Unfortunately, many of these physicians do not look for signs of mental illness in their patients, he said.
“Unless [general practice physicians] provide depression screening, most of these cases are missed because of their focus on physical health care,” Miller said.
Depression was measured in the NHANES using the Patient Health Questionnaire (PHQ-9), a nine-item screening instrument that asks questions about the frequency of symptoms of depression over the two weeks prior to the interview. Depression was defined as a PHQ-9 score of 10 or higher, a well-validated cutoff point commonly used in clinical studies that measure depression, according to the CDC authors.
The CDC analysis of the NHANES is posted at<www.cdc.gov/nchs/data/databriefs/db07.htm>.▪



