Care for Vets, Active Military Focus of APA Advocacy Effort
How can veterans' families gain access to the mental health services offered to former soldiers? When will the government agree on the need for a bigger boost in the number of Department of Veterans Affairs (VA) and Department of Defense (DOD) psychiatrists? What will it take for the federal government to increase treatment reimbursement to private psychiatrists who participate in the military's health care network?
Those were among the most-discussed questions and most-lobbied issues during APA's 2008 Advocacy Day.
The annual event, held last month, drew about 100 psychiatrists to Washington, D.C., to learn about the biggest federal health policy challenges facing psychiatry and to urge their members of Congress to support APA-backed solutions. Attendees participated in several days of training and heard multiple issue updates before visiting the offices of members of Congress from 44 states, which is an increase from the 40 states whose representatives were reached in last year's Capitol Hill visits.
This year's advocacy issue updates focused on the mental health needs of active-duty members of the military and veterans. Health care services for members of the military and veterans have had large funding increases in recent years to help remedy inadequate services that have long existed. Especially damning was the revelation of poor medical conditions at Walter Reed Army Medical Center in Washington, D.C. But the federal agencies have placed less emphasis on improving mental health care, and the Advocacy Day participants hoped to change that.
Veterans health issues are among the few issues in Washington on which there is bipartisan agreement, “so feel comfortable raising them during your visits to Capitol Hill and with the knowledge that you bring great expertise to the issue,” said Ralph Ibson, J.D., vice president of Government affairs at Mental Health America, to the psychiatrists participating in Advocacy Day.
The participants raised numerous concerns about the shortcomings of the DoD and VA mental health system—such as an inadequate medical workforce—that they were encouraged to share with their congressional representatives during their legislative visits.
Dan Blazer, M.D., Ph.D., said the heavy caseloads, poor compensation, and frequent overseas duty had decimated the ranks of mental health professionals in the military. The military needs to focus resources on recruitment of active-duty personnel to fill those positions instead of increasing its use of contract workers, he said.
Kelly Hruska, deputy director of the Department of Government Relations at the National Military Family Association, agreed that more effort is needed to increase access to mental health professionals in both the military and VA systems.
“The biggest concern is access to providers,” Hruska said.“ Families know that services are out there; they just don't know how to find providers that accept TRICARE.”
TRICARE is the health care program that serves primarily active-duty service members, National Guard and Reserve members, retirees, and their families worldwide. TRICARE brings together the health care resources of the military and supplements them with networks of civilian health care professionals and institutions.

William Callahan, M.D., chair of the Committee on Public Affairs and a member of APAPAC, talks to fellow psychiatrists during the annual event.
Credit: Ellen Dallager
Psychiatrists in private practice repeatedly pointed out that more of them would participate in TRICARE if it reimbursed at a higher rate or entailed less-onerous paperwork. The program reimburses clinicians at rates significantly below those of Medicare, and remuneration frequently takes more than one year to receive, they said.
Although such changes are needed to encourage more psychiatrists to care for this population, veterans groups and government officials praised psychiatrists for already contributing significant assistance through programs such as Give an Hour (Psychiatric News, March 7). The program, supported by APA, is a growing network of mental health professionals and psychiatrists who commit to giving one hour a week for at least a year to soldiers, veterans, and their family members seeking help through the program.
Another area of mental health care that psychiatrists attending Advocacy Day frequently mentioned as needing congressional action is the lack of access veterans' families have to most VA health care services.
“Right now the focus is on family care to the extent that it helps the veteran, but it doesn't address the separate care that the families need who don't have a direct service connection,” said Ira Katz, M.D., deputy chief of patient care services officer for mental health in the VA.
Katz noted that it would take an act of Congress to allow the VA to provide the same level of health care to veterans' families that it now provides to veterans.

Meeting attendees include Elizabeth LeQuesne, M.D., a member of the Committee on gay, Lesbian, and Bisexual Issues (left) and Sherry Katz-Bearnot, M.D., president of the American Academy of Psychoanalysis and Dynamic Psychiatry.
Credit: Ellen Dallager
Attendees and speakers during the Advocacy Day program also urged steps to smooth the mental health care transition for soldiers as they leave the military and its health system and become eligible for VA care.
Blazer and others urged better coordination of electronic medical records to make them accessible to both the military and VA health systems. A staff aide said that the member of Congress for whom he works plans to introduce such legislation.
Legislation that addresses another concern—how to get veterans to seek and continue needed mental health treatment—was introduced in the Senate in January and was hailed by several APA members. The Veterans Mental Health Treatment First Act (S 2573) would pay veterans who are diagnosed with posttraumatic stress disorder (PTSD) and other serious mental health conditions and who follow the prescribed treatment.
“There is the fear that if you are less than perfect, then it ends your career,” said APA President Carolyn Robinowitz, M.D., about the stigma many members of the military fear will follow treatment for an emotional problem or psychiatric illness.
Transitioning Smoothly From DoD to VA
James Peake, M.D., secretary of the VA, agreed with Advocacy Day participants that there are many areas in which his department can improve the mental health care it provides, including reducing the stigma some fear from mental health treatment and the provision of a smoother transition from the DoD to the VA health care system.
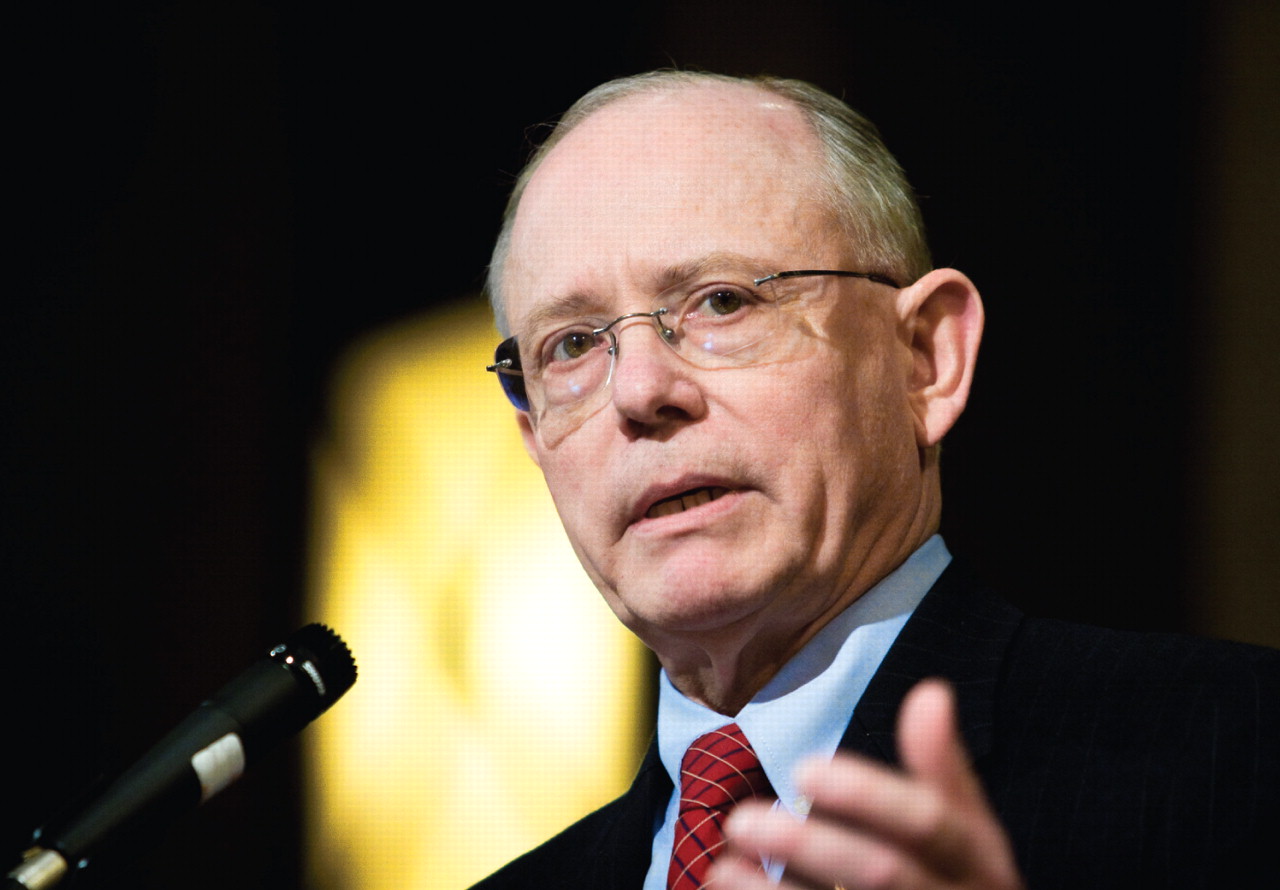
James Peake, M.D., secretary of the Department of Veterans Affairs, tells Advocacy Day attendees about federal efforts to improve the mental health care provided to veterans and members of the military.
Credit: Ellen Dallager
“There is no reason that the transition between DoD and the VA can't be seamless, and that has to be more than a buzzword,” he said, in comments to attendees.
Peake said the development of an electronic medical record that both systems can use is critical to that seamlessness. Further, advancing health information technology and conducting more research on traumatic brain injury (TBI) are other leading priorities of his department, he said.
Recent advances at the VA include an extension from two years to five years the period in which combat veterans can access VA care, which would provide more time to identify and treat individuals for TBI and PTSD. Another advance is that all returning service members are screened for suicidal tendencies and TBI, with detailed evaluations made when the screening results are positive. Ongoing research at the VA also seeks to better tailor the PTSD care to the needs of recent combat veterans, compared with the type of treatment needed by older Vietnam combat veterans.
Peake noted that the VA has stepped up its suicide prevention efforts after its leaders were “shocked” by the high number of suicides among recent veterans under their care. These efforts included a national suicide prevention hotline for veterans, which has been credited with preventing more than 400 suicides to date, and placement of suicide prevention coordinators in all VA medical centers (Psychiatric News, September 7, 2007).
Better care is needed for veterans' families as well, Peake said. He noted, however, that his department is largely limited by federal law in the care it can provide.
“The 1945 reality has changed, and many more members of the military and veterans are now married,” Peake said.
Members' Efforts Recognized

R. Dale Walker, M.D., chair of the Council on Advocacy and Public Policy, (left) presented the President's Special Recognition Award to Jeffrey Akaka, M.D., for his legislative efforts on scope-of-practice issues in Hawaii. Also pictured is Lori Murayama, M.D., secretary-treasurer of the Hawaii Psychiatric Medical Association.
Credit: Ellen Dallager
Also at the Advocacy Day event, participants recognized the special advocacy accomplishments of several individuals, including Jeffrey Akaka, M.D., speaker of the APA assembly. He was presented the President's Special Recognition Award for his leadership in the successful lobbying effort to stop state legislation in Hawaii that would have granted prescribing privileges to psychologists.
“A Crash-course prescribing practice passed both the House and Senate, and it looked dark [for us],” Akaka said. “We did not give up.”
The governor eventually vetoed the bill, and Akaka and other psychiatrists encouraged the legislature not to override it.
“They are tall shoulders on which I have stood to get to this place,” Akaka said. “The shoulders of all you here are what our members will stand on.”
The Advocacy Day event was also a success in reaching APA's goal of increased lobbying participation by members-in-training. Twenty-five residents attended the 2008 event, up from 20 last year and 10 in 2006. (For more on Advocacy Day see Original article: Advocacy has Maximum Impact When we all Speak up and Original article: First Advocacy Day Whets Appetite for More.)
Information about the Veterans Mental Health Treatment First Act can be accessed at <http://thomas.loc.gov:> by searching on the bill number, S 2753.▪



