How Does Brain Produce Emotions? International Team Seeks Answers
Thinking about how emotions arise and are processed by the brain has traditionally looked something like the blind men contemplating the elephant, according to University of Sydney professor of cognitive neuroscience Leanne Williams, Ph.D., director of the Brain Dynamics Centre of the Westmead Millennium Institute.
Existing models are monodimensional, defined by scientific disciplines, even as the contemporary study of brain, behavior, body, and genetics is colliding, she reminded listeners at the annual meeting of the American Psychosomatic Society in Baltimore in March.
Better to step back and consider the process as a whole, she said.“ What is common across these theories? What can we learn by looking across disorders?”
Williams and others in BRAINnet, a consortium of researchers on four continents studying the brain and mental health, seek to develop an integrative neuroscience that combines psychological and cognitive tests of emotion—like responses to facial displays of emotions—with technical studies like EEGs or MRIs. Together, they should provide good time and spatial resolution to show when and where the response to an emotional event takes place in the brain.
So far, BRAINnet has garnered data from 5,000 healthy subjects and 1,000 clinical subjects.
Looking at the brain this way in health and illness might also provide insights into psychiatric conditions, she said.
“There are no psychiatric disorders that don't have a fundamental disorganization of emotional brain organization,” said Williams. She begins her inquiry by asking: “What is the purpose of emotions?”
Her answer begins with evolution. She recalled that Darwin studied facial expressions of emotion and said they were remnants of previous survival traits.
“The fundamental principles of evolution are avoiding danger and maximizing safety or reward,” she said. “Emotional cues relevant to those principles will be the most significant and have the greatest survival value, and thus will drive brain organization. Emotion is more than a feeling—it's an 'action tendency.' ”
Signs of danger represent a “mismatch” to the emotional brain and prompt high psychological arousal. Mismatches are stimuli that are unpredictable, loud, unexpected, asymmetrical, or usually external or have high visual contrast. A “match” signals safety and is predictable, familiar, and symmetrical. Matches and mismatches can also be seen as having high or low intensity (arousal) and a positive or negative significance.
The brain gives priority to mismatch cues for threats, since they have higher evolutionary survival value.
Match/mismatch cues lie on a continuum and have their effect in a very brief time—milliseconds to start with. Threat signals function in the 0 to 150 ms range, not through cortical sensory pathways but by way of the brainstem directly to the amygdala. Damage to this “feeling” network can be seen in people with lesions in the amygdala, who show deficits in recognizing fear.
A mismatch induces familiar flight/fight reactions: heart rate and blood pressure increase, pupils dilate, and more blood flows to the brain. A match causes increased blood flow to the body, lowers blood pressure, constricts the pupils, and slows the heart rate.
About 300 ms marks the transition from reaction to awareness, when the stimulus converts to emotion. Beginning at 500 ms, the brain starts to draw on memory to appraise the initial arousal. Over subsequent minutes and hours, the cumulative outcomes can play a role in neural plasticity. Spatially, signal processing moves from the brainstem to the prefrontal cortex.
Until recently the conventional view held that emotional processing had to be preceded by conscious awareness of the stimulus. Williams said that the combination of neuropsychiatric tests and imaging studies indicates the opposite.
“Significant emotions may be processed without conscious awareness, within the first 150 ms,” she said.
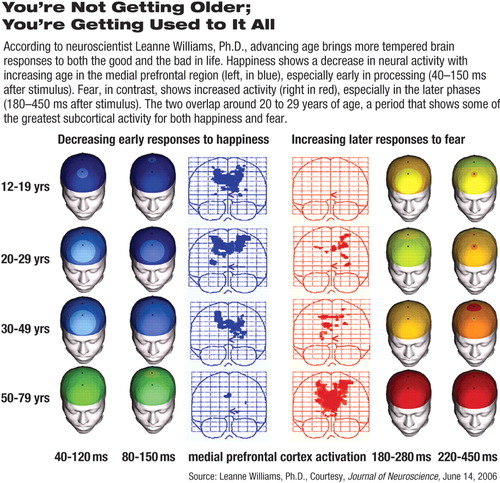
In addition, there is a shift with gender and age, she noted. Women seem more sensitive to threats than men. Also, both men and women display a later response to fear as they grow older, meaning they get better at regulating fear. But they also exhibit a decreased early response to happiness.
These patterns indicate a trend among older people to greater emotional stability and less emotional intensity.
(Williams and her colleagues refer to old age as “the mellow years.”)
The integrative neuroscience model may also offer insights into psychiatric illness and suggest research directions, said Williams.
For instance, depressed patients show a slower and more varied reaction time to sadness when reading faces, while patients with anxiety show a slowed reaction time to explicit fear but a faster response to implicit fear. A disorder such as posttraumatic stress disorder seems to reflect a heightened early response to mismatch cues, but with less prefrontal evaluation and regulation later on, as seen in healthy controls.
The breakdowns in perception and thought that are part of schizophrenia may reflect an inability to distinguish between match and mismatch cues and process information appropriately, she suggested.
“These are crucial in making predictions about functioning in the real world, at work, or in personal relationships. The brain is not dealing well with arousal and feedback,” she said.
In anorexia nervosa, reward-related cues—in this case for food—are processed as if they were mismatch cues. They trigger neural networks for danger and are not fully normalized with weight gain. Subjects with ADHD exhibit poor emotion recognition mismatches that are not differentiated from noise.
The next stage in this area of research will include studying genetic polymorphisms associated with changes in brain function and perhaps biological markers that will relate the biological to the behavioral. Ultimately, such research may lead to better treatment support decisions and medications, said Williams.
A recent article in The Neuroscientist by Williams and Evian Gordon, “Dynamic Organization of the Emotional Brain: Responsivity, Stability, and Instability,” is posted at<http://nro.sagepub.com/cgi/reprint/13/4/349>.▪



