Psychiatrists Are Helping Their Patients Get Care
In early April, APA surveyed its members about the impact of the current economic crisis on their patients and practices. A total of 805 members responded.
Although only 18 percent of respondents reported that the economic crisis was having a substantial impact on the mental health of their patients, 70 percent said that because of the crisis their patients were having to choose between psychiatric care and other basic needs.
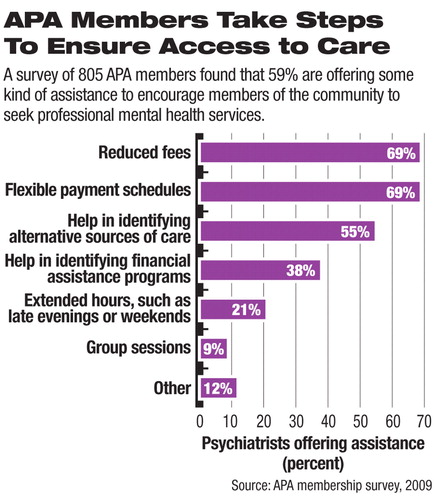
Fifty-nine percent of respondents also said that they were taking steps to help such financially strapped patients get needed care (see chart). One method was reducing fees. Another was structuring flexible payment schedules. Still a third was referring them to alternative, less expensive sources of care. Interviews that Psychiatric News conducted with members illustrate some of the steps that they are taking in this regard.
“A lot of my job now is trying to help patients pay for things,” said Leigh White, M.D., who works in a student psychiatry service at Michigan State University. “I try to stretch their visits to help them reduce costs.”
“I have had consultations that I have had to refer out because people have been concerned about how much money [a psychiatrist visit] is going to cost,” reported Hunter McQuistion, M.D., director of outpatient and community psychiatry at St. Luke's and Roosevelt Hospitals in New York City.
“I encourage patients not to quit treatment, not to take a hiatus, so that they won't backslide or relapse,” said Rosalind Griffin, M.D., a psychiatrist in private practice in Farmington Hills, Mich. “I tell them that I am willing to let them pay as they are able to.... [I also try to convince them that] talking about their inability to pay, their guilt, and their shame about being in debt is more therapeutic than staying away from therapy in order to not increase their debt.... They need their ego strength to get through this really critical period.”
“I had one patient with bipolar disorder who was on an atypical antipsychotic,” Daniel Dahl, M.D., an associate professor of psychiatry at the University of Alabama, said. “He had trouble affording his medication and stopped taking it. So we put him in the hospital, where he could afford it.”



