More Med Students Choose Psychiatry, Reversing Recent Year Declines
The number of U.S. medical school graduates entering PGY-1 psychiatry residency slots this year increased by 10 percent over last year, according to data from the National Resident Match Program (NRMP).
A total of 656 U.S. graduates chose psychiatry, up from 595 last year. The increase reverses three years of slight declines that began in 2005.
As a percentage of the total number of U.S. seniors who matched into residency positions in any specialty this year (14,566), however, those matching into psychiatry has remained stable over several years at 4.5 percent.
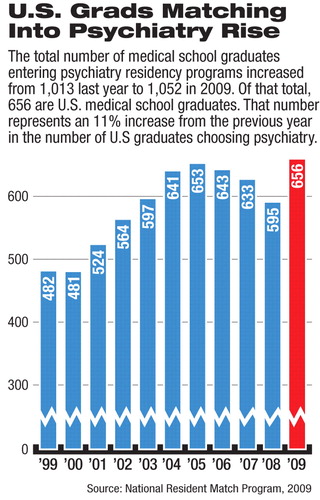
As in past years, international medical graduates (IMGs) continue to be critical to the larger picture of psychiatry's emerging workforce: in addition to the 656 positions filled by U.S. graduates, 396 first-year residency positions were filled mostly by IMGs (a small number are filled by U.S. graduates who didn't graduate this year). Altogether, 1,052 positions were filled, or 99 percent of those that were offered. That total figure is up from 1,013 in 2008.
“We at APA are pleased at the continued increase in psychiatry positions filled through the match,” commented Deborah Hales, M.D., head of APA's Division of Education. “Advances in our science, more flexible practice options, and patient need all make psychiatry an attractive choice.”
David Kaye, M.D., incoming president of the American Association of Directors of Psychiatric Residency Training, told Psychiatric News,“ The good news is that we are holding our own and growing a little bit. I'd like to think there is a lot of excitement today about being a psychiatrist. Our treatments are better and better established, and there is less stigma.”
He noted especially that only 11 positions went unfilled this year.“ Not too long ago we had hundreds of unfilled slots,” he said.
Regarding the continued heavy reliance on international graduates, Kaye said, “Most of us believe the country needs a lot more psychiatrists. So we need IMGs to come in and fill that public-health need.”
The results of the annual match, reflecting the specialty choices of physicians who will be in practice for the next 30 to 40 years, are looked at like tea leaves for clues to the shape of medicine in the future. Five specialties experienced a 10 percent or greater increase in the number of U.S. graduates choosing the specialty since 2005: anesthesiology, emergency medicine, obstetrics-gynecology, plastic surgery, and radiology. Surgery and internal medicine have experienced equivalent declines.
APA Trustee Sidney Weissman, M.D., who has long taken an interest in workforce issues, said he believes that efforts at health system reform—which likely will have an impact on physician earnings—are bound to be a factor in shaping psychiatry's future workforce.
“Career selection or matches in future years, I believe, will be greatly impacted by the outcome of the proposed reorganization of the American health care system,” Weissman stated. “It is argued that our country's current health care expenditures can be reduced by one-third without loss of quality and with a concurrent expansion to the uninsured.
“Whether true or not, we can anticipate changes in how our health care services are structured, which may or will impact on physician incomes,” he said. “Proposals exist to alter the current physician payment system. This may or will lead to changes in our current fee-for-service models and could either positively or negatively impact on psychiatry.
“In light of the degree of indebtedness of graduating U.S. medical school seniors, any perceived or real changes in potential incomes of specialties will likely impact on their career choices.”
The match, conducted annually by the NRMP, uses a computer algorithm to align the preferences of applicants with the preferences of residency program directors to fill the thousands of training positions available at U.S. teaching hospitals each year.
The NRMP is a private, not-for-profit organization established in 1952 to provide an orderly and fair mechanism for matching residents with residency programs.
The NRMP is sponsored by the American Board of Medical Specialties, American Medical Association, Association of American Medical Colleges, American Hospital Association, and Council of Medical Specialty Societies.
More information on this year's match results are posted at<www.nrmp.org/>.▪



