Building 'Medical Homes' Among Leading Health Reform Proposals
Extensive changes are needed in the payment systems for physicians and other clinicians as part of health care reform, say physician leaders who met with members of the Obama administration at a physician forum in March.
“We need major change in the payment system,” said APA Medical Director James H. Scully Jr., M.D., who attended a White House physician health care reform meeting in March. “Physicians want to be paid for doing the right thing for their patients” (Psychiatric News, April 17).
Under current reimbursement approaches, physicians are frequently caught between efforts to control costs and improve quality, with little attention given to long-term health care outcomes on which clinicians are focused.
“You don't have to pay us for everything we do,” said AMA President Nancy Nielsen, M.D., at a forum sponsored by the Alliance for Health Care Reform in March. “On the other hand, when you deliberately don't pay us for some things, it does send a pretty powerful message.”
Numerous options have been proposed to reinforce the goal of many reformers that physicians should be focused on long-term health.
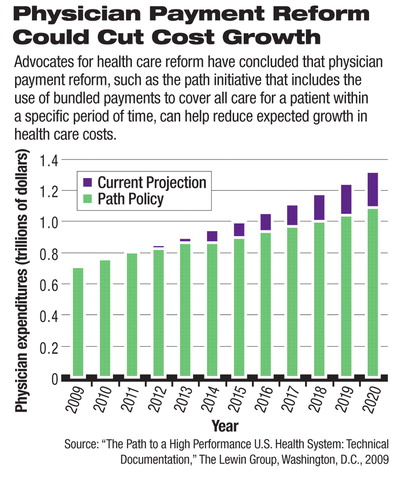
Among prominent payment reform approaches that have been proposed by physician advocates and health policy experts are increasing the compensation for primary care, using bundled payments to cover care over a specified period of time, and offering clinicians financial incentives to serve as“ medical homes” for patients and coordinate care among all the clinicians treating a particular patient.
With regard to increased compensation, much of the payment reform debate has been focused on what many experts view as the powerful disincentives that current payment systems create for physicians to provide primary care. The long-standing, low reimbursement for primary care has been linked to the shrinkage of that area of medicine as a percentage of medical fields and to declining numbers of medical students going into primary care, according to physician leaders.
The current payment structure impacts psychiatrists in a similar manner, Scully said, because their health care services—like those of primary care physicians—are relatively low cost and do not drive increases in overall health care costs “but are not well paid.”
Another prominent approach to payment reform is to extend physician use of“ bundled payments” that already are given to hospitals as a per-patient “case rate.” Such bundled payments are given as lump sums to clinicians for care they provide to a patient over a set period of time.
A report on health care payment reform released in February by the nonpartisan Commonwealth Fund suggested revising the Medicare fee schedule to boost primary care payments and add annual increases. The Commonwealth Fund report and other reform studies also have advocated broad adoption of the medical-home model to encourage more accessible, coordinated, patient-centered care that focuses on long-term health promotion and disease prevention.
Medicare's medical-home pilot projects improved communication with patients through phone calls and secure e-mail and offered benefits such as improved patient self-management skills, said Robert Berenson, M.D., a senior fellow at the Urban Institute and former director of Medicare payment policy and private health plan contracting at the Centers for Medicare and Medicaid Services (CMS). Medical homes also have improved communication with other physicians and community-based services that provide care for their patients, he said. However, such care-coordination services are difficult to track and are unlikely to work in fee-for-service payment systems, which generally do not reimburse for that work, Berenson noted.
“We need to move from the fee-for-service system that dominates our health care now to payment systems that reward taking broader accountability for patient outcomes and care and also for high performance in terms of efficiency as well,” said Stuart Guterman, assistant vice president of the Commonwealth Fund's Program on Medicare's Future and former director of the Office of Research, Development, and Information at CMS.
The benefits of a medical-home approach are expected to especially benefit people with serious mental illness, who often have co-occurring nonpsychiatric illness and require long-term, chronic disease care. APA has urged CMS to expand its medical-home project to include psychiatrists as the coordinating physician of patients with serious mental illness and co-occurring nonpsychiatric health problems. Pilot programs by CMS explicitly bar psychiatrists serving patients as their medical homes.
The greatest benefits for both clinicians and patients ultimately may come from a combination of the various payment reforms under consideration, according to physician leaders and reform advocates.
“In the end, we need to consider doing hybrids of all of these approaches,” said Berenson, a leading Medicare expert. “Each has its strengths and weaknesses.”
For instance, Berenson said medical homes that improve care coordination for patients with chronic conditions could be reimbursed as a monthly per-patient fee, while individual office visits could still be based on fee-for-service charges.
Implementing such a hybrid approach nationwide could be problematic, said Bruce Hamory, M.D., executive vice president and chief medical officer emeritus at Geisinger Health System in Pennsylvania.
“Whether you can in fact do that with a piece of legislation for the country as a whole is a different matter,” Hamory said. He urged that physician groups or “other accountable organizations” decide specific reimbursement combinations based on the economics of specific regions or localities.
Hybrid reimbursement systems also could use pay-for-performance approaches, which are popular with many health reform leaders in Congress, to try to avoid unintended side effects, such as undertreatment.
Regardless of whether a hybrid or a new single-payment system is devised, the AMA's Nielsen urged caution in any changes undertaken in health care payment reform.
“We think that there may be a problem if it's a one-size-fits-all, immediate shift in payment,” she said.
The Commonwealth Fund study “Reforming Provider Payment: Essential Building Block for Health Care Reform” is posted at<www.allhealth.org/briefingmaterials/CMWFreformingproviderpayment-1423.pdf>.▪



