States Address Diverse Issues Affecting Mental Health Care
Abstract
Several states have recently enacted laws or regulations that could affect people who have mental illness.
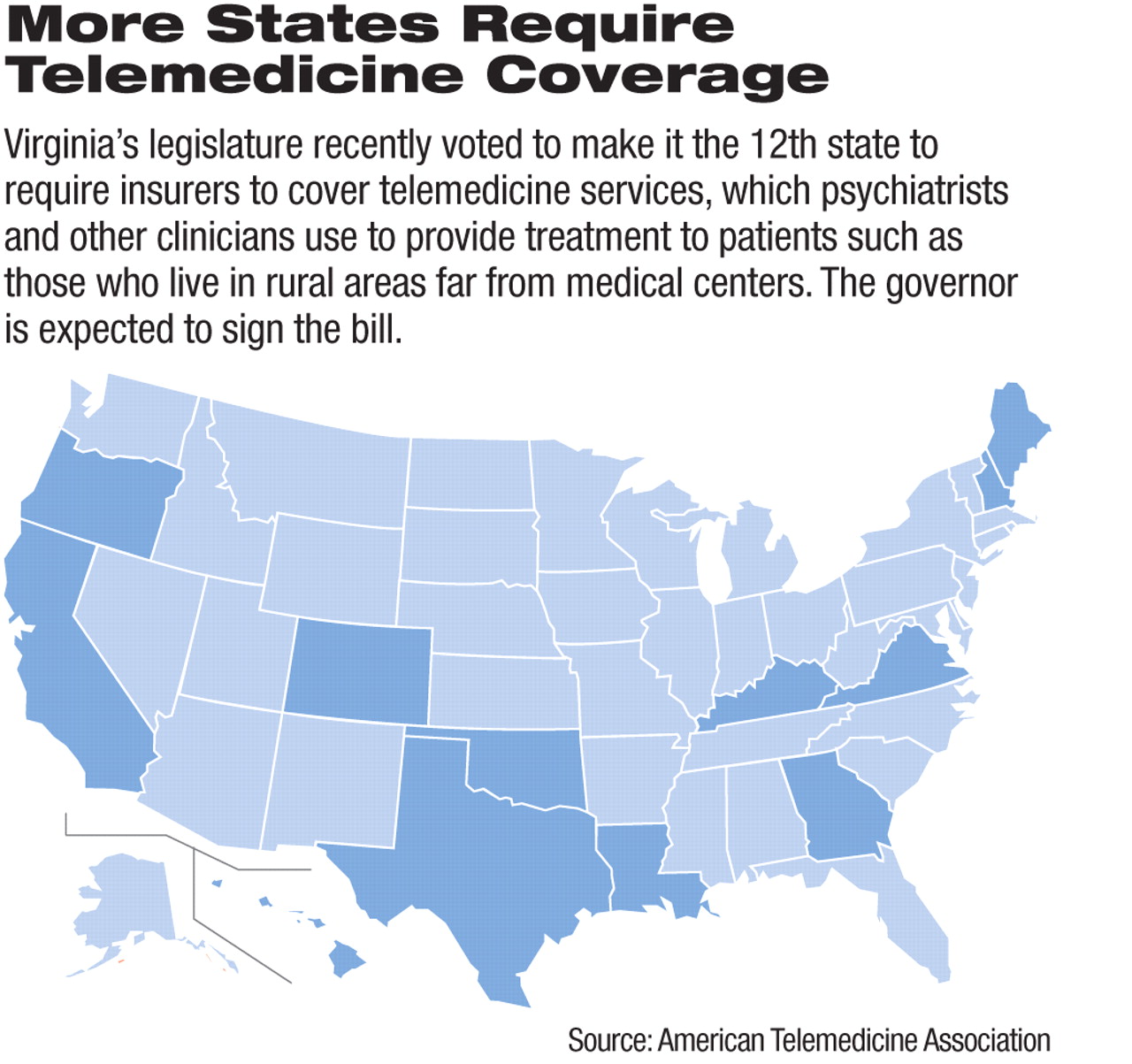
• The Virginia legislature added a requirement that health care insurers in the state cover telemedicine services, which are increasingly used by psychiatrists to treat patients living in rural areas.
The legislature's March approval of a telemedicine coverage requirement (SB 675) would make Virginia the 12th state to require health insurers to cover the use of a wide variety of remote treatments. Gov. Bob McDonnell (R) is expected to sign the measure, according to supporters.
In addition to covering telemedicine services for mental health care, including “counseling,” the bill would require coverage of such services as use of university-based digital networks, remote cardiac monitoring, and home-care monitoring of patients with advanced diabetes.
Mental health uses are “a very major part of where telemedicine is going,” said Jonathan Linkous, CEO of the American Telemedicine Association (ATA), in an interview with Psychiatric News.
He noted that many psychiatrists and mental health clinicians already use phone or video technology to provide some therapy and clinical updates to patients.
The ATA has recognized the large mental health role in telemedicine by issuing practice guidelines for videoconference-based therapy, which were developed in cooperation with APA and other mental health organizations.
Many insurers in Virginia and other states are already moving to cover telemedicine because of the cost-effectiveness of its treatments, Linkous said. So the legislation is generally considered a “final push” to get widespread adoption of such coverage.
The change would bring Virginia into line with the other states that have mandated telemedicine coverage: California, Colorado, Georgia, Hawaii, Kentucky, Louisiana, Maine, New Hampshire, Oklahoma, Oregon, and Texas.
Information on the ATA's telemedicine practice guidelines is posted at <www.americantelemed.org/i4a/pages/index.cfm?pageid=3311>.
• In Vermont, the state's insurance regulator recently issued a requirement that insurance companies that cover the loss of college tuition due to unforeseen circumstances include psychiatric illnesses. The new requirement applies a 1997 state law mandating parity coverage for physical and mental health to insurers that reimburse tuition payers for their loss if the student is unable to complete the schooling for which he or she has already paid. The ruling followed a complaint by a Vermont college student about a company's failure to adhere to the state's insurance parity law.
The complaint questioned the legality of insurers' refunding only 60 percent of students' college tuition when they leave due to mental illness but 100 percent when they leave due to physical disability.
This reimbursement disparity issue has taken on a growing urgency during the recession as more families seek to recover tuition when their child has to leave college, according to media reports. Tuition insurers indicate that up to 10 percent of parents buy such insurance, which is often sold through the university at which a student is enrolled.
The impact of mandating parity coverage could have a significant effect, because high rates of alcohol abuse and other psychiatric illnesses are characteristic of college-student populations and may require leaves of absence to treat. The most prevalent psychiatric disorders in college students are alcohol use disorders (20.37 percent of students) and personality disorders (17.68 percent of students), according to an analysis of federal survey data reported in the December 2008 Archives of General Psychiatry.
Information on the mental health impact of tuition reimbursement insurance in Vermont is available from the Vermont Association for Mental Health at <www.vamh.org>.
• The administration of Florida Gov. Charlie Crist (R) has proposed expanding a controversial Medicaid pilot program by up to 19 counties. The initiative, which will be considered by the state legislature in its current session, would require up to 375,000 Medicaid beneficiaries in those jurisdictions to enroll in private-sector managed care plans.
Because the expansion could save $58.7 million in the new fiscal year, Crist is touting it as a cost-saving effort to help close the state's likely $1 billion budget gap. The cost saving, supporters maintain, would come from managed care plans' ability to reduce fraud and hold down spiraling Medicaid costs through strict utilization review and other measures.
The pilot program, which operates in Broward, Duval, Baker, Clay, and Nassau counties, drew criticism from researchers over its impact on people with psychiatric illnesses. A 2008 study of the pilot program by Georgetown University's Health Policy Institute concluded that the program's use of private managed care plans was frequently a poor fit for beneficiaries with serious psychiatric conditions. The researchers suggested that the state take a more active role in ensuring that Medicaid beneficiaries receive the types and levels of mental health services they need.
The legislature also is considering numerous cuts to mental health and substance abuse programs in the state of as much as $172 million.
• California's legislature is considering a range of substantial mental health care cuts as part of its effort to close a massive budget deficit. The state would close 327 adult health care centers throughout California to save $135 million in Fiscal 2011.
The cuts have drawn criticism from health care advocates, who warn that many of the 37,000 low-income patients at the centers suffer from brain injuries, dementia, and other chronic conditions and will end up costing the state even more money if the centers close. Many untreated patients will likely end up in publicly supported nursing homes or be hospitalized at state expense as their conditions deteriorate.
Another proposed cut of $811 million, or 40 percent, from the state prison health care budget has gained some popular support but could run into opposition from federal courts, which have taken over the state's prison health care system after lawsuits were brought alleging systemwide failures to provide inmates with needed care. 



