Which Disorders Rank Highest on the Misery Meter?
Abstract
Of all the mental disorders that can afflict people, which inflict the greatest misery?
Some of the affective disorders, data from two related studies show.
The first study was published in the April 2007 British Journal of Psychiatry, the second in the November 2010 issue of that journal.
The lead investigator was Samuli Saarni, M.D., Ph.D., a senior researcher at the National Institute for Health and Welfare in Helsinki, Finland.
In the 2007 study, the researchers screened a representative sample of about 8,000 Finns in medical settings using the Composite International Diagnostic Interview (CIDI) to determine whether, during the past year, they had been diagnosed with major depressive disorder, dysthymia, panic disorder, social phobia, agoraphobia, general anxiety disorder, or alcohol dependence.
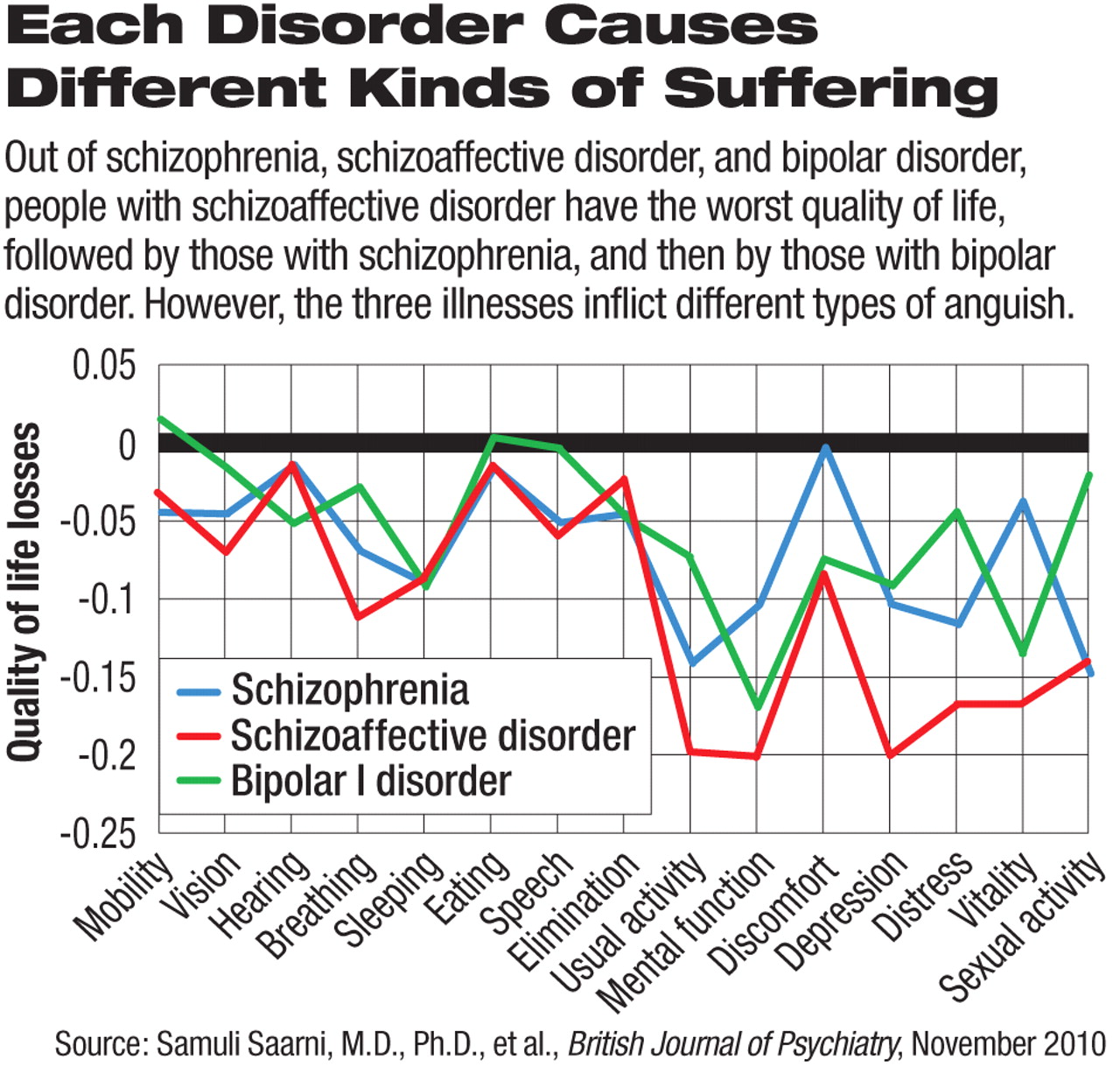
The researchers then evaluated individuals who had such disorders with an instrument called the Health-Related Quality of Life 15D (HRQoL 15D), which was developed by Harri Sintonen, a professor of health economics at the University of Helsinki, in 1981. It rates 15 dimensions of an individual's quality of life. These are mobility, vision, hearing, breathing, sleeping, eating, speech, elimination, usual activities, mental function, discomfort, depression, distress, vitality, and sexual activity.
Those with dysthymia, general anxiety disorder, agoraphobia, or social phobia were found to have the worst quality of life among the surveyed sample.
In the 2010 follow-up study, the researchers also screened the same sample of some 8,000 Finns using the Structured Clinical Interview for DSM-IV (SCID-1) to determine whether any of them had schizophrenia, schizoaffective disorder, or bipolar disorder. The HRQoL 15D was again used to evaluate the quality of life in those found to have one of these disorders.
Among those with one of these three disorders, those with schizoaffective disorder were found to have the worst quality of life, followed by those with schizophrenia, and then by those with bipolar disorder.
Finally the researchers compared the quality-of-life findings for those individuals who had dysthymia, general anxiety disorder, agoraphobia, or social phobia with those for subjects who had schizoaffective disorder, schizophrenia, or bipolar disorder. They found that those with anxiety disorders or dysthymia suffered even more than those with the three more severe disorders did.
Specifically, quality-of-life according to the HRQoL 15D findings were -0.13 to -0.14 for individuals with dysthmia, general anxiety disorder, agoraphobia, or social phobia; -0.09 for individuals with schizoaffective disorder; -0.06 for individuals with schizophrenia; and -0.05 for individuals with bipolar disorder.
Fifteen aspects of quality-of-life made up each of these totals. How did each contribute to the totals? Saarni told Psychiatric News that it was difficult to answer, “as in our two papers we actually only compared the HRQoL patterns within each group of conditions (psychotic or nonpsychotic), not between them.”
In any event, Saarni said, “Most striking to me has been the large impact of anxiety disorders and dysthymia, all of which have traditionally been considered neurotic, milder conditions. Anxiety disorders especially have not been high treatment priorities in comparison to depression, even though good evidence-based pharmacological and psychological treatments exist [for the anxiety disorders]. For example, the World Health Organization/World Bank burden-of-disease studies did make the impact of depression well known, but failed to include most anxiety disorders.”
Saarni said that he also was surprised, but in a positive direction, “by the relatively good subjective quality of life of patients with schizophrenia in contrast with their more objective functioning.” Or, he explained, he was really not surprised by the findings insofar as they conformed with his clinical experience, but he was surprised by the findings insofar as they contradicted the public's generally dismal view of schizophrenia. He thus hopes that these results will help reduce the stigma that people with schizophrenia often encounter from the public.
The study was funded by the Finnish National Institute for Health and Welfare.
An abstract of “Impact of Psychiatric Disorders on Health-Related Quality of Life: General Population Survey” is posted at <http://bjp.rcpsych.org/cgi/content/abstract/190/4/326>. An abstract of “Quality of Life of People With Schizophrenia, Bipolar Disorder, and Other Psychotic Disorders” is posted at <http://bjp.rcpsych.org/cgi/content/abstract/197/5/386>.



