Burgeoning Field of Study Could Impact Psychiatry
Abstract
The field of psychoneuroimmunology, which started a quarter-century ago, is vigorously moving ahead, experts in the field report (see How Several Psychiatrists Became Interested in Psychoneuroimmunology).
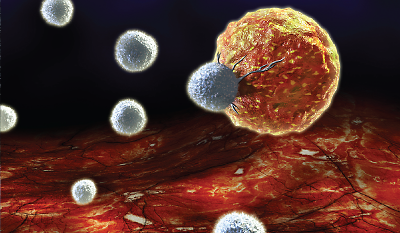
T cells—shown here attacking a cancer cell—appear to be important to brain function, psychoneuroimmunologists are learning.
It is being turbocharged by several factors, Michael Irwin, M.D., a professor of psychiatry at the University of California, Los Angeles (UCLA), explained in an interview. “One is that science is becoming increasingly interdisciplinary and transdisciplinary, and psychoneuroimmunology has been in that forefront now for two decades. Psychiatrists, psychologists, and behavioral scientists are working hand in hand with neuroscientists, neuroendocrinologists, and immunologists. Second, there have been tremendous advances in the technologies that we have available.”
For example, scientists can now survey the activity of the entire human genome—all 22,000 or so human genes—as they act in cells of the immune system, Steven Cole, Ph.D., a professor of medicine at UCLA, pointed out.
All this momentum is leading to valuable discoveries, psychoneuroimmunologists agree.
“One is the role that adversity—particularly long-term adversity such as chronic threat or uncertainty—plays in activating some parts of the immune system even as it shuts down other parts,” Cole said. “For instance, while T-cell antiviral responses and B-cell antibody responses are often suppressed, first-line defense responses to tissue injury that are involved in inflammation, such as pro-inflammatory cytokines, are actually up-regulated.”
“Very closely related to that, I think, is the finding that psychosocial stress is really a pro-inflammatory state,” Charles Raison, M.D., an associate professor of integrative mental health at the University of Arizona, noted. “Some people get more inflammatory reactions than others. There is now consistent evidence that when you expose people who had experienced early-life adversity to a psychosocial stressor, they experience robust inflammatory responses. But even folks without adversity, if they respond to stress, their blood pressure goes up, their heart rate increases, and they’ll experience a bump in circulating cytokines.”
Still another important finding about psychosocial stress is that its impact on the heart is just as great as other known cardiovascular risk factors such as high cholesterol, smoking, and lack of physical activity, Irwin pointed out.
T Cells Tell Surprising Tale
And yet another valuable discovery, according to Andrew Miller, M.D., a professor of psychiatry at Emory University, occurred when researchers took mice that had been genetically designed not to have any T cells and found that the mice were incapable of learning. The researchers then gave the mice T cells via bone-marrow transplants and found that they could learn after that.
“This tells us that T cells are playing a fundamental role in the ability of the brain to learn and process information and that the immune system may play a larger role in brain function than we ever realized,” he said.
“This may be the most important psychoneuroimmunology discovery of the past decade,” Raison declared.
And these discoveries have psychiatric implications, psychoneuroimmunologists point out.
For instance, it’s not short-term exposure to stress, but long-term exposure to it that ultimately plays havoc with the immune system and leaves people vulnerable to disease, Cole said. “One bad day doesn’t seem to be terribly threatening to your health. What is really bad are one hundred or a thousand bad days—a lifestyle of threat or uncertainty.”
Another finding with psychiatric implications, Raison explained, is that “if inflammation makes you depressed—and there is some good evidence for this—one might predict that treating people who are depressed with an anti-inflammatory regimen might have some clinical benefit. And there are early studies to suggest this.…”
“There [also] seems to be a unique association between being treatment resistant as far as depression is concerned and increased levels of inflammatory cytokines,” Miller pointed out. “So the more inflammation you have, the less likely you are to respond to antidepressants. And many of the things that are associated with depression-treatment resistance, like obesity, early life stress, anxiety disorders, and medical illnesses, are all associated with increased inflammation.”
“We now likewise know that sleep disturbance can increase inflammation and the risk of depression,” Irwin added. “So treatments that specifically target sleep disturbance reap promise as a means to decrease the risk of developing a depression. This is a big paradigm shift for psychiatrists. For many decades we focused only on the treatment of depression. But these data from the field of psychoneuroimmunology suggest that we can look at people at risk for depression and target the underlying biology to decrease the risk of actually developing depression in the first place.”
Greater Impact to Come
And as the field charges ahead, it should have an even greater impact on psychiatry.
For example, psychoneuroimmunologists know that if you give people cytokines, it makes them depressed. So “I think we will learn whether blocking cytokines is a good antidepressant strategy, and if so, what the best cytokine to block is,” Raison said. “And the question of whether it is going to show a general effect or whether it is only going to be useful for people who have chronically elevated inflammation, that, I think, we will know. I think we will also learn to what degree T cells’ ability to impact cognitive and emotional functioning offers promise for the treatment of psychiatric conditions.”
Finally, “since the immune system is now known to influence brain function, I think we are going to learn whether manipulation of the immune system can alter neurodevelopmental disorders such as autism,” Miller suggested. “And since immune-system inflammation is now known to be involved in neurodegenerative diseases such as Alzheimer’s and Parkinson’s, I think we are going to see whether immune-system manipulation can counter such diseases.” 
How Several Psychiatrists Became Interested in Psychoneuroimmunology
“As a psychiatrist, I was once asked by an oncologist to see a patient who was receiving a cytokine called interferon alpha for malignant melanoma,” Andrew Miller, M.D., a professor of psychiatry at Emory University, recalled during an interview. “The reason why is because the patient was depressed. I was expecting to see someone who was very sick and was surprised to meet a pleasant middle-aged woman, and she proceeded to describe to me how a strange feeling had overcome her since taking this cytokine. She loved her husband, she loved her children, and there were so many things she loved to do, like gardening. But now she couldn’t stand to be with her husband and children, and she no longer wanted to garden. She cried at the drop of a hat. ‘I’ve completely come to grips with the cancer,’ she said. ‘That’s not what’s bothering me.’ ”
“What was so surprising,” Miller continued, “was that she was describing a classic case of major depression, yet there was no psychological reason for it. This was an extremely profound experience for me. I began to realize that these immune molecules—these inflammatory cytokines—could have powerful effects on how people think and feel.”
“I was trained in internal medicine and became convinced that many of the patients I was seeing in internal medicine had significant psychological stressors that had impacted their risk for developing diseases,” Michael Irwin, M.D., a professor of psychiatry at the University of California, Los Angeles, told Psychiatric News. “I started reading about the influence of stress on health and learned that the immune system, which is a primary player in pathology in all these diseases, was not being actively studied as a potential mechanism that would underlie the impact of stress on these health outcomes. So in 1982, while a resident in psychiatry, I started examining the impact of significant loss—of a husband—on immune measures that were important in disease risk.”
“I initially got interested in the field because I was trying to study advanced Buddhist meditators,” Charles Raison, M.D., a psychiatrist and an associate professor of integrative mental health at the University of Arizona, recalled. “Their meditation practices tapped into bodily pathways that sort of forced the brain into certain emotional states. So I realized that if we could come to understand what those men were doing, it might cast some light on why people get stuck in emotional states like depression.”



