Social and Work Skills Keys to BPD Recovery
Abstract
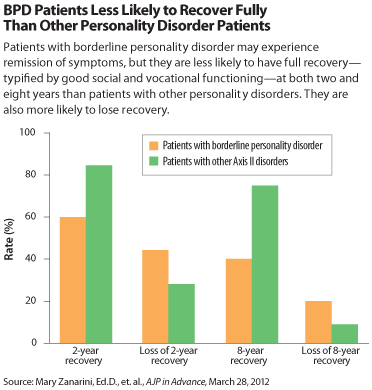
Remission of symptoms of borderline personality disorder (BPD) is quite common with treatment, but long-term recovery—typified by remission plus good social and vocational functioning—is much less so.
Moreover, patients with BPD over time fare worse in terms of remission, recurrence of illness, recovery and loss of recovery than do patients with other personality disorders.
Those were the major findings of a longitudinal comparison of BPD and other personality disorders that was posted online on March 28 in AJP in Advance.
The study, by Mary Zanarini, Ed.D., and colleagues at McLean Hospital in Belmont, Mass., confirm and extend the conclusions from a similar study by the same group that appeared in the American Journal of Psychiatry in 2010: that a substantial number of patients with BPD experience symptomatic remission, but that recovery—requiring social and concurrent vocational functioning—is much less common. That report, “Time to Attainment of Recovery From Borderline Personality Disorder and Stability of Recovery: A 10-Year Prospective Follow-Up Study,” did not include the Axis II comparison group and was restricted to looking at remission at two years and four years and recovery at two years.
The new study looks at remission and recovery at eight years and adds nuance to the severity of BPD by showing that patients with other forms of personality disorder fare better on all measures.
“The Axis II comparison group does better than BPD patients across the board,” Zanarini told Psychiatric News. “Long-lasting remissions are very common in both groups, and recurrences of symptoms, though more common among BPD patients, are low in both groups. The longer patients in both groups are remitted the lower the chance of recurrence for both. So there is good news for BPD patients—while they are functioning more poorly than patients with other personality disorders, they are still functioning well in the symptomatic realm. It’s when you look at recovery, involving not only remission of symptoms but also good social and vocational functioning, that the two groups really start to separate.”
In the study, 290 inpatients with BPD and 72 comparison subjects with other Axis II disorders were assessed during their index admission using a series of semi-structured interviews, which were administered again at eight successive two-year follow-up waves.
Remission was defined as no longer meeting study criteria for BPD or another personality disorder for two years or longer. Recovery was defined as meeting a Global Assessment of Functioning score of 61 or higher, with at least one emotionally sustaining relationship with a close friend or life partner/spouse and the ability to work or go to school consistently, competently, and on a full-time basis.
By the time of the 16-year follow-up assessment, the cumulative rates of remission for borderline patients ranged from 78 percent for those with an eight-year remission to 99 percent for those with a two-year remission. The corresponding rates for those with another personality disorder were 97 percent and 99 percent, respectively.
Cumulative rates of recovery for borderline patients ranged from 40 percent for recoveries lasting eight years to 60 percent for recoveries lasting two years. For Axis II comparison subjects, cumulative rates of recovery ranged from 75 percent for recoveries lasting eight years to 85 percent for recoveries lasting two years.
Rates of recurrence of symptoms were higher for BPD patients at both time points as well, and patients with BPD also experienced recurrence of symptoms more quickly (see chart).
Zanarini emphasized that the results call for more of a rehabilitation-model of treatment that includes vocational training for BPD patients who have achieved long-term symptom remission. She said lower rates of recovery than remission for patients with BPD over time is largely due to deficits in vocational function.
“Patients have a lot of trouble getting and holding on to a full-time job,” she said. “That’s typically not something clinicians have paid attention to or are even looking for their BPD patients to attain. But we strongly suggest that when someone reaches the stage where they are stable and remitted for a long period, they need rehabilitation that focuses on vocational function,” Zanarini said. “No one enjoys just staying at home.”
The study was funded by grants from the National Institute of Mental Health. 
“Attainment and Stability of Sustained Symptomatic Remission and Recovery Among Patients With Borderline Personality Disorder and Axis II Comparison Subjects: A 16-Year Prospective Follow-Up Study” is posted at http://ajp.psychiatryonline.org/Article.aspx?ArticleID=1065354.



