Topiramate Could Be Considered First Line Treatment for AUD, Study Suggests
Abstract
The study adds to a now voluminous literature showing that medication is useful for treating patients with alcohol use disorder (AUD).
Topiramate appears to be at least as effective as naltrexone in reducing heavy alcohol consumption and superior to naltrexone in reducing total alcohol consumption, according to a randomized, controlled comparison of the two medications in the May American Journal of Psychiatry (AJP). Naltrexone is regarded as the first-line treatment for alcohol use disorder (AUD).
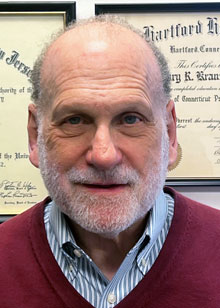
“One could make an argument on the basis of data in [the American Journal of Psychiatry study] that clinicians should start with topiramate,” said study co-author Henry Kranzler, M.D.
Topiramate was also found to be more effective than naltrexone at reducing craving, as measured by the Penn Alcohol Craving Scale, and on serum gamma glutamyl-transferase (gGT), an objective blood measure of alcohol consumption.
“Both medications reduced self-reported alcohol consumption with a clear overall treatment response observed in the first week of treatment,” wrote lead author Kirsten Morley, Ph.D., professor, specialty of addiction medicine, at the University of Sydney, and colleagues. “However, we found significantly greater effects of topiramate in the pattern of alcohol consumption.” She is the Director of the Addiction Treatment Research Theme at the Edith Collins Centre, Specialty of Addiction Medicine at Royal Prince Alfred Hospital.
A total of 147 patients with AUD (average age 47, 39% female) were randomly assigned to receive topiramate up to a maximum dosage of 200 mg/day or naltrexone at 50 mg/day for 12 weeks. Patient response to both drugs was stratified according to the presence of two genetic polymorphisms that had been previously shown to affect treatment response—one in the GRIK1 gene, which encodes a glutamate receptor subunit, and the other in OPRM1, which encodes the mu-opioid receptor.
The primary outcome was the number of heavy drinking days (HDD) per week, defined as five or more drinks per day for men and four or more drinks per day for women; secondary outcomes included mean standard drinks per drinking day (SDDD, or the number of drinks consumed on a day when the individual drinks), body mass index (BMI), craving, markers of liver injury, mood and adverse events.
Patients receiving topiramate experienced a greater (though nonsignificant) decrease in heavy drinking days per week than those treated with naltrexone: During the last week of treatment, the naltrexone group experienced 33% more heavy drinking days than the topiramate group. The topiramate group also reported a more significant decrease in the number of drinks per drinking day than the naltrexone group—during the last week of treatment, the naltrexone group reported an average of 1.15 more drinks per drinking day than those receiving naltrexone.
At week 12, the topiramate group had a greater reduction in the Penn Alcohol Craving Scale score from baseline (17.1 to 10.1) than the naltrexone group (17.2 to 12.2) and a greater reduction in gGT concentration; the topiramate group also had a significantly greater reduction in BMI. The study tested the effect of two genetic polymorphisms on treatment response to the drugs but found no effect.
Study co-author Henry Kranzler, M.D., a professor of psychiatry and director of the Center for Addiction Studies at the University of Pennsylvania’s Perelman School of Medicine, said topiramate is becoming more widely used for AUD, though it remains an off-label treatment, while naltrexone is FDA approved. He noted, for instance, that AUD treatment guidelines from the Veterans Administration recommend topiramate as a first-line treatment, in contrast to APA’s guideline. APA’s practice guideline on the treatment of patients with AUD recommends use of topiramate or gabapentin for patients who are “intolerant of or do not respond to naltrexone or acamprosate.”
“I recommend treating a patient with AUD with naltrexone initially because it is easy to use, can be taken once a day, and is well tolerated,” Kranzler told Psychiatric News. “For patients who don’t respond well to naltrexone, I recommend topiramate. However, one could make an argument based on data in [the AJP study] that clinicians should start with topiramate.”
He said side effects are more common with topiramate—paresthesia, mental “fogginess,” changes in taste—but the study found that withdrawal due to side effects was uncommon for both drugs (8% and 5% of the topiramate and naltrexone groups, respectively.)
Kranzler said the significantly greater reduction in average drinks per drinking day and the non-significant reduction in heavy drinking days week are important measures of clinical improvement, even if effect sizes were not large.
The finding that neither of the genetic polymorphisms affected treatment response is telling, he continued. “In view of recent genetic findings, it is a little simple-minded to think that single nucleotide polymorphisms, which have very small effects by themselves, will predict something complex like treatment response,” he told Psychiatric News. “We need to look at more powerful measures of genetic effects in larger samples.”
Most important, Kranzler said the AJP study adds to a now voluminous literature showing that medication is an effective treatment for AUD. “Neither naltrexone nor topiramate is prescribed very often,” he said. “I suspect it has to do with the fact that in our society alcohol use disorder is generally viewed as a failure of will or a bad habit—a lethal one but not one that is amenable to pharmacotherapy.”
He said he is currently conducting a study of extended-release naltrexone; when patients complete the study, they often want their physician to prescribe naltrexone—but physicians often refuse because they don’t want to prescribe a drug with which they are unfamiliar, Kranzler said.
Possible remedies for the undertreatment of AUD include incorporating more medical student instruction on the medication treatment of patients with substance use disorders and training other health care professionals on the identification and treatment of patients with these disorders. “We need to create a climate that recognizes addiction as a medical problem for which there are medical treatments,” he said.
The study was supported by a grant and Fellowships from the National Health and Medical Research Council of Australia. ■



