Your Patient Has Mixed Features. Now What?
Abstract
The pharmacological options are similar for unipolar and bipolar patients presenting with mixed features with the important exception of frontline antidepressant use.

The mixed features modifier was introduced with DSM-5 to allow clinicians to more accurately diagnose and treat patients who may be experiencing concurrent symptoms of depression and mania/hypomania. Still, mixed features remain underappreciated and undertreated. To effectively treat a patient with mixed features, you must first recognize the presence of these symptoms and the underlying disorder.
It is important to understand that mixed features are not limited to bipolar disorder. A patient is considered to have mixed features if they show depressive symptoms during periods of mania or hypomania, but also if there is a presence of mania in individuals with bipolar depression or major depressive disorder (MDD).
Once identified correctly, the next challenge is treating a disorder that is characterized by more severe illness, higher rates of comorbid conditions such as substance use disorder or obesity, and a lower response to therapy than a non-mixed mood state (1). While studies to date have yet to point to a definitive method for treating patients with mixed features, the Florida Medicaid Guidelines for Mixed Features, developed in 2015, offer one evidence-based strategy (2,3; see accompanying chart below).
The Florida guidelines were specifically developed for patients with MDD and mixed features, but the pharmacopeia for a mixed features diagnosis is similar for patients with bipolar disorder, with one critical exception: the use of antidepressants.
Mood destabilization is a known risk when treating patients experiencing manic or hypomanic symptoms with antidepressants. Nonetheless, the panel helping to shape the Florida guidelines concluded that not enough evidence was available in patients with MDD and DSM-5-defined mixed features to forbid the use of conventional antidepressants. Thus, antidepressant monotherapy is considered one of the three first-line treatment options for major depression with mixed features. In patients with bipolar disorder and mixed features, treatment with antidepressants is not endorsed. There is a lot of debate in the bipolar research community on the appropriate use of antidepressant therapy for bipolar patients (4), but in the case of mixed features the risks of mood destabilization are significant.
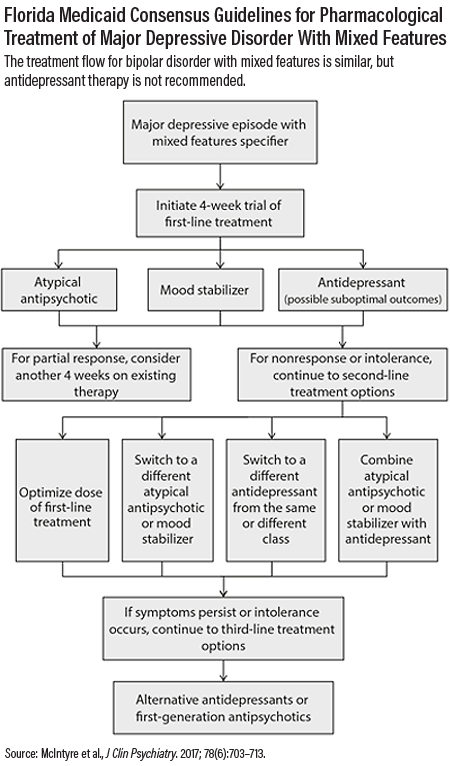
Other first-line therapies outlined in the Florida guidelines include mood stabilizers, such as lithium or lamotrigine, and second-generation antipsychotics. The evidence for the use of mood stabilizers for mixed features is limited, but lithium may be useful to alleviate aggression or suicidality (5). Among antipsychotics, quetiapine may be a preferred choice, though weight gain is a common side effect. Lurasidone is promising since it has been reported to have fewer metabolic side effects, but so far, the evidence of effect is limited to one clinical study of patients with unipolar depression (6) and one post-hoc analysis of patients with bipolar depression (7).
Whatever you prescribe, be prepared for a patient with mixed features to fail to respond to monotherapy. If there are no changes in symptoms after four weeks on monotherapy, a dose increase or an adjunct medication might be needed. In the case of a partial response, consider continuing monotherapy for an additional four weeks.
If a patient still fails to respond after trying adjunctive therapies, drug switching, and/or dose optimization attempts, third-level options include electroconvulsive therapy, transcranial magnetic stimulation, alternative antidepressants such as tricyclics or monoamine oxidase inhibitors, or first-generation antipsychotics such as haloperidol.
To maximize the chance of symptom improvement for this often-refractory illness, these medication guidelines should be part of a comprehensive therapeutic plan. Proper sleep hygiene, lifestyle changes, and behavioral therapies should all be discussed as components for recovery. ■
1. Perugi G, Quaranta G, Dell’Osso L. The Significance of Mixed States in Depression and Mania. Curr Psychiatry Rep. 2014;16(10):486.
2. McIntyre RS, Suppes T, Tandon R, et al. Florida Best Practice Psychotherapeutic Medication Guidelines for Adults With Major Depressive Disorder. J Clin Psychiatry. 2017;78(6):703–713
3. Florida Medicaid Drug Therapy Management Program for Behavioral Health. 2015 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults. University of South Florida. Sponsored by the Florida Agency for Health Care Administration. December 2015.
4. Pacchiarotti I, Bond DJ, Baldessarini RJ, et al. The International Society for Bipolar Disorders (ISBD) Task Force Report on Antidepressant Use in Bipolar Disorders. Am J Psychiatry. 2013;170(11):1249–1262
5. Song J, SjɆlander A, Joas E, et al. Suicidal Suicidal Behavior During Lithium and Valproate Treatment: A Within-Individual 8-Year Prospective Study of 50,000 Patients With Bipolar Disorder. Am J Psychiatry. 2017 Aug 1;174(8):795-802.
6. Suppes T, Silva R, Cucchiaro J, et al. Lurasidone for the Treatment of Major Depressive Disorder With Mixed Features: A Randomized, Double-Blind, Placebo-Controlled Study. Am J Psychiatry. 2016;173(4):400–407.
7. McIntyre RS, Cucchiaro J, Pikalov A, et al. Lurasidone in the Treatment of Bipolar Depression With Mixed (Subsyndromal Hypomanic) Features: Post Hoc Analysis of a Randomized Placebo-Controlled Trial. J Clin Psychiatry. 2015;76(4):398–405



