Substance-Induced Psychosis Associated With Later Schizophrenia, Bipolar Disorder
Abstract
The rate of conversion to schizophrenia or bipolar disorder was found to be a remarkable 47.4 percent for those who have an incidence of cannabis-induced psychosis.
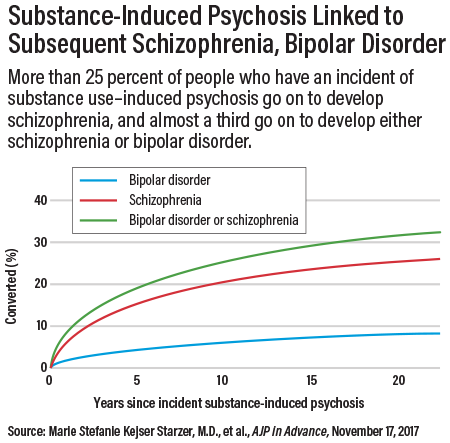
As many as a third of all patients with substance-induced psychosis may go on to develop schizophrenia or bipolar disorder within five years, according to a report posted November 28, 2017, in AJP in Advance. The highest conversion rate was found for cannabis-induced psychosis, with 47.4 percent converting to either schizophrenia or bipolar disorder.
The findings suggest the need for early identification and rapid treatment. “It is important to diagnose new cases of schizophrenia and bipolar disorder as soon as possible and to initiate treatment without delay, because prolonged psychosis without treatment is associated with a worse prognosis,” wrote Marie Stefanie Kejser Starzer, M.D., and colleagues at Copenhagen University Hospital.
Starzer and colleagues analyzed data from the Danish Psychiatric Central Research Register, which has registered all inpatient psychiatric treatment since 1969 and outpatient treatment since 1995.
The study population consisted of 6,788 patients who received a diagnosis of substance-induced psychosis over a 20-year period and who did not have any previous record of treatment for schizophrenia spectrum disorders or bipolar disorder. Ten comparison subjects were selected for each case subject, matched on sex, year, month of birth, and being alive at the date of the incident substance-induced psychosis of the corresponding case subject.
The case subjects were followed up from incident substance-induced psychosis, and comparison subjects from their corresponding match date, until the first occurrence of schizophrenia or bipolar disorder or until death, migration, or August 14, 2014, whichever came first.
A total of 32.2 percent of all patients with substance-induced psychosis converted to either schizophrenia or bipolar disorder. In addition to cannabis use, self-harm after a substance-induced psychosis was significantly linked to a higher risk of converting to schizophrenia or bipolar disorder. Young age was associated with a higher risk of conversion to schizophrenia; the risk was highest for those aged 16 to 25 years.
Fifty percent of conversions to schizophrenia occurred within 3.1 years, and 50 percent of conversions to bipolar disorder occurred within 4.4 years. “Based on the different risk factors identified in different analyses and the overall conversion rate of 32.2 percent, it seems most reasonable to suggest that all patients with a substance-induced psychosis should be offered follow-up,” the authors stated. The follow-up period from incidence of substance-use induced psychosis should be at least two years, they wrote.
Psychiatrist John McGrath, M.D., whose research has focused on modifiable risk factors for schizophrenia, told Psychiatric News that the findings are consistent with expectations—substance use disorders can precede more persistent mental disorders like schizophrenia and bipolar disorder.
McGrath noted that the findings in the current study are correlational and cannot be construed to mean that substance use causes schizophrenia or bipolar disorder. “Some of the temporal sequence may be causal—research has consistently shown a small causal effect. But we are always careful about inferring causation from correlational research.”
He is the Niels Bohr Professor at Aarhus University, Denmark, and conjoint professor at the University of Queensland, Queensland Brain Institute. (McGrath said he works in Denmark half-time and is acquainted with the authors, but he was not consulted on the AJP study).
McGrath pointed out another reason that follow-up is important: people with apparent substance-induced psychosis may progress to other disorders, not just schizophrenia or bipolar disorder.
Deepak D’Souza, M.D., a professor of psychiatry at Yale University School of Medicine, agreed that the study adds to a growing literature suggesting that substance-induced psychosis, and in particular cannabis-induced psychosis, may be a harbinger of a chronic psychotic disorder.
“That young people are more vulnerable to developing a chronic psychotic disorder following an episode of substance-induced psychosis is not surprising given what is known about the vulnerability of the developing adolescent brain to drugs, and specifically cannabis,” he told Psychiatric News.
D’Souza said schizophrenia is believed by many to be heterogenous, encompassing a number of subtypes, and suggested that schizophrenia resulting from substance use may be a distinct subtype.
He also said clinicians may be encountering more substance-induced psychosis. “With the growing legalization of medical and recreational cannabis, it is not unreasonable to assume that young people are more likely to be exposed to cannabis and that some of them who are vulnerable, for reasons we don’t fully understand, may experience a cannabis-related psychosis,” he said. “If such a large number of individuals with a clinically significant substance-induced psychosis episode develop a serious mental illness such as bipolar disorder or a chronic, recurrent psychotic disorder, then mental health systems should offer and encourage long-term follow-up to such individuals at the time they first present with a clinically significant substance-induced psychosis episode.” ■



