Health Plans Appear to Have Expanded Services Post-Parity Passage
Abstract
APA staff say that patient access to care is still negatively impacted by nonquantifiable treatment limitations.
Behavioral health care services have expanded since the enactment of the Federal Mental Health Parity and Addiction Equity Act (MHPAEA)—at least on paper.
More than two-thirds of insurance products offered in the private market expanded behavioral health coverage, according to a survey of commercial health plan executives published January 16 in Psychiatric Services. Moreover, slightly more than half of executives surveyed said cost sharing for behavioral health services decreased, according to the report by Dominic Hodgkin, Ph.D., and colleagues at the Institute for Behavioral Health at the Brandeis University Heller School for Social Policy and Management.
Hodgkin and colleagues said that the self-report by health plan executives—unverified by independent sources—suggests that, on the whole, plans appear to have responded as intended to MHPAEA. “We did not find evidence either of widespread noncompliance or of the unintended effects that some had feared, such as dropping coverage of behavioral health care altogether,” they stated.
Hodgkin and colleagues conducted telephone surveys from September 2010 to June 2011 and August 2014 to April 2015 with executive-level directors at private health plans or with “a person most knowledgeable about behavioral health service delivery.” For both 2010 and 2014, they examined the percentage of members with behavioral health coverage, the percentage of products excluding coverage of specific diagnoses, the percentage of products covering certain specific services, types of cost sharing, and the percentage of products requiring prior authorization for in-network outpatient general medical and behavioral health care.
In 2014, 274 plans responded (80 percent) and reported on 705 products. Respondents said 68 percent of insurance products had expanded behavioral health coverage. A little more than half (54 percent) responded that behavioral health cost sharing had decreased since 2010. In contrast, general medical cost sharing was described as having decreased in only 2 percent of products.
A majority of respondents reported that their prior-authorization policies remained unchanged for both behavioral health (57 percent) and general medical care (65 percent).
APA staff monitoring compliance with the parity law said that the results are commendable—if not surprising—but added that the survey doesn’t address a range of nonquantifiable treatment limitations, especially issues related to provider reimbursement, stricter review of medical necessity, and network adequacy that affect patient access.
The authors themselves acknowledged this weakness of the survey, noting that in at least one prior survey of patients, 29 percent reported that they or their family member had been denied mental health care on the basis of medical necessity. “Managed care techniques appear to result in more complaints than do benefits issues, perhaps reflecting the greater difficulty of monitoring plan policies in this area,” Hodgkin and colleagues stated. “Gaps in plans’ provider networks are also cited as a problem.”
Irvin “Sam” Muszynski, J.D., APA’s senior policy advisor and director for parity implementation and enforcement policy, told Psychiatric News that the study confirms that in general financial limitations on mental health and substance use disorder services have improved, and the scope of coverage has remained steady.
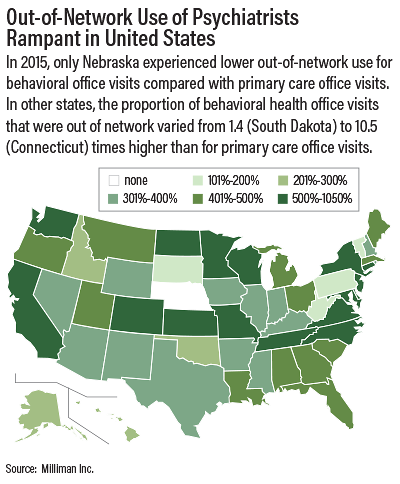
But he said expanding coverage is meaningless if patients cannot access care because there are too few providers in plan networks. “What the study does not capture is the simultaneous movement by the plans to lower reimbursement rates across the board to behavioral health providers, driving narrower networks,” he said. “It doesn’t capture lower in-network participation, dramatic increases in out-of-network utilization (if patients have the coverage and can afford it), and gaming of medical necessity criteria that overall are negative to the patient access envisioned by the parity law.”
Milliman Inc. issued a study late last year that found that psychiatrists are paid significantly less than general medical and surgical physicians providing the same or similar services and that patients’ use of out-of-network services is extremely high for behavioral health compared with general medical and surgical services (see map).
Muszynski said APA staff continue to monitor implementation of parity and to work with federal and state insurance regulators to improve compliance. ■
“Federal Parity and Access to Behavioral Health Care in Private Health Plans” can be accessed here.



