EDs Seeing More Patients Who Abuse Medications
In 2005 there were 108 million visits to emergency departments (EDs) in U.S. hospitals, and an estimated 1.5 million of these visits were associated with drug misuse or abuse, according to U.S. government data.
Drug Abuse Warning Net works (DAWN) researchers gathered data from 355 emergency rooms across the United States by reviewing medical records related to recent drug use. To be included in the analysis, drugs needed only to be implicated in the visit; they did not have to be the cause of the visit.
All data were estimated using weighted calculations based on actual visits to emergency departments.
Emergency department visits linked to the nonmedical use of medications increased more than 20 percent from 2004 to 2005, according to the government's DAWN report, “National Estimates of Drug-Related Emergency Department Visits,” issued by the Substance Abuse and Mental Health Services Administration in March.
According to the data, 598,542 emergency department visits involved nonmedical use of prescription or over-the-counter drugs or dietary supplements.
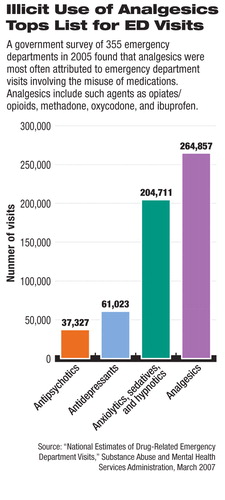
Opiates and opioid analgesics accounted for 33 percent of the visits linked to nonmedical use of medications and included hydrocodone/combinations (51,225 visits), oxycodone/combinations (42,810 visits), methadone (41,216 visits), and fentanyl/combinations (9,160 visits).
Antianxiety agents, including benzodiazepines, accounted for 34 percent of these visits (172,388 visits).
When government researchers examined trends among drug-related emergency visits from 2004 to 2005, they found that reports involving benzodiazepine use increased by 19 percent, those involving opiates increased by 24 percent, and methadone-related visits increased by 29 percent.
Over half (56 percent) of all drug misuse or drug abuse emergency department visits involved an illegal drug either alone or in combination with another drug type—cocaine was involved in 448,481 visits, marijuana in 242,200 visits, heroin in 164,572 visits, and stimulants (including amphetamines and methamphetamines) in 138,950 visits.
In 2005, 816,696 emergency visits involved use of an illicit drug, either alone or with another type of drug.
The DAWN data also showed that 492,654 emergency visits involved the use of alcohol, of which 98,430 involved alcohol only for patients under age 21, and 394,224 visits involved both alcohol and drugs for patients of all ages.
When researchers looked at data for drug-related suicide attempts, they found that there were 132,582 emergency room visits for such attempts in 2005, and in nearly two-thirds (63 percent) of them multiple drugs had been used.
The report's authors noted that all suicide attempts involving drug use were captured by the data, even when patients used weapons, for example, in the attempt.
More than half of the visits for drug-related suicide attempts involved psychotherapeutic agents, with the most common types being benzodiazepines and antidepressants. About 45 percent of the suicide attempts involved central nervous system agents such as prescription and over-the-counter analgesic medications.
“Drug Abuse Warning Network, 2005: National Estimates of Drug-Related Emergency Department Visits” is posted at<oas.samhsa.gov/DAWN/2k5ed.cfm>.▪



