Surgeon General Decries Large Gaps In Children’s Mental Health System
The U.S. Surgeon General released an ambitious national agenda last month to improve children’s mental health and their ability to have access to the care they need when they develop mental health problems.
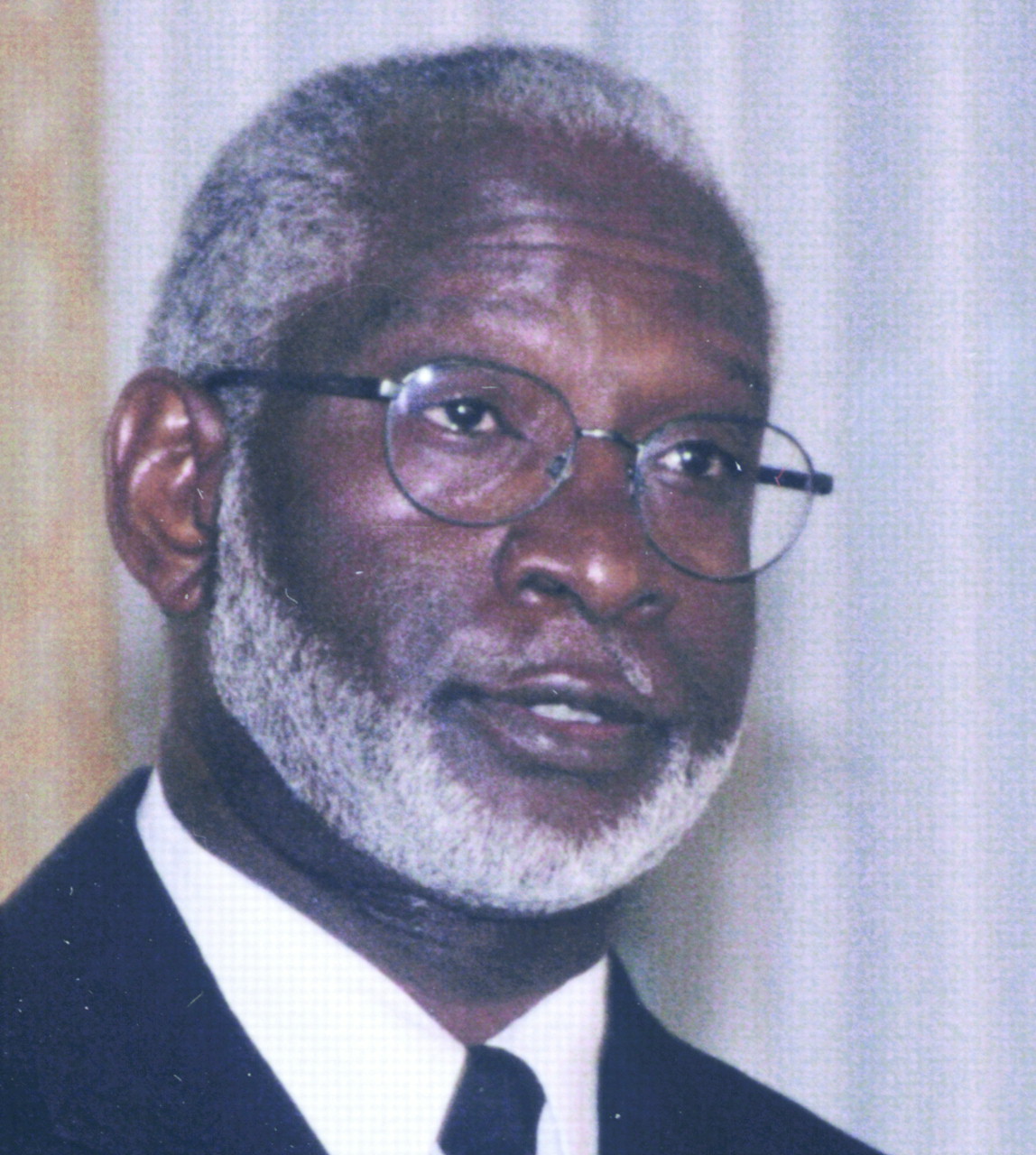
Surgeon General David Satcher, M.D.: “Growing numbers of children are suffering needlessly.”
“Growing numbers of children are suffering needlessly because their emotional, behavioral, and developmental needs are not being met by the very institutions and systems that were created to take care of them,” said Satcher in a press release.
His “blueprint for change” identifies eight goals and multiple action steps. These include improving detection and assessment of mental illness, eliminating stigma, and improving access to and coordination of mental health services. The surgeon general also calls for more research on preventing and treating children’s psychiatric disorders and increased efforts to disseminate the findings to mental health and other health care providers.
David Fassler, M.D., chair of the APA Council on Children, Adolescents, and Their Families, commented to Psychiatric News, “We welcome the report and applaud the surgeon general’s commitment to improving awareness of child psychiatric disorders and advocating for enhanced access to comprehensive assessment and individualized treatment.”
The report is based on recommendations from the surgeon general’s September conference on children’s mental health (Psychiatric News, October 20, 2000) and an October meeting on psychopharmacology for young children sponsored by the U.S. Food and Drug Administration and the National Institute of Mental Health.
The report advocates educating families about mental illness to improve early recognition in children. “We need to help families understand that the problems are real, that they can be prevented, and that effective treatments are available,” said Satcher. The report does not specify who the surgeon general expects to conduct this family education effort.
Primary care providers, teachers, school counselors and coaches, and clinicians in all disciplines also need more education about mental illnesses to improve detection, said Satcher.
Kelly Kelleher, M.D., a Staunton professor of pediatrics and psychiatry at the University of Pittsburgh School of Medicine, stated in the report that primary care physicians are becoming more knowledgeable about mental illnesses but still encounter many barriers to appropriate assessment and treatment.
These obstacles include parents underreporting behavioral and emotional problems, the requirements that office visits be brief, insurance restrictions, and a lack of available child mental health specialists, thus delaying referrals, according to Kelleher. More than two-thirds of primary care clinicians who pursue a referral for a child patient report encountering appointment delays, with average time to appointment with a specialist being three to four months. Of those patients who were referred, 59 percent had no visits to the specialist; only 13 percent averaged one or more visits a month in the follow-up period of six months. In short, an increasing number of problems (15 percent to 30 percent) are being identified by primary care providers, but rates of recognition (48 percent to 57 percent) are still low, and connections to mental health specialists are difficult.
Because many people, especially the poor and minorities, lack health insurance or have substantial insurance restrictions, the surgeon general’s national agenda advocates for comprehensive and universal health coverage.
Rep. Marge Roukema (R-N.J.) referred to the surgeon general’s recommendation when she reintroduced the Mental Health and Substance Abuse Parity Act on January 3, which would mandate that psychiatric and substance abuse disorders receive the same insurance coverage as physical disorders (Original article: see page 2).
The recommendation to expand research on children’s psychiatric disorders and disseminate the findings to mental health and other health care practitioners was also applauded by APA and patient advocacy groups.
“While progress has been made in developing treatments for children’s mental disorders, a huge gap remains between the findings and the everyday practices of all mental health disciplines that treat children,” said psychiatrist Peter Jensen, M.D., director of the Center for the Advancement of Children’s Mental Health.
There is also a need to disseminate accurate information about evidence-based treatments, said Jensen, who contributed to the surgeon general’s report and serves as a professional advisory board member to the organization Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD).
“For example, many people don’t realize that 69 percent of children with ADHD have a co-occurring illness including bipolar, anxiety, obsessive-compulsive, depressive or tic disorders, and that multimodal treatment is very effective,” said Jensen in a press release.
APA will continue to work with members of Congress and the Bush administration to advance the goals outlined in the surgeon general’s report, according to APA President Daniel Borenstein, M.D.
Other psychiatrists who participated in the child mental health conference and other activities that led up to the new report include Steven Hyman, M.D., director of NIMH; Bernard Arons, M.D., director of the Center for Mental Health Services; Mary Jane England, M.D., president of the Washington Business Group on Health and a former APA president; Kenneth Wells, M.D., of the psychiatry department at UCLA; and Carl Bell, M.D., president and CEO of the Community Mental Health Council in Chicago.
The “National Action Agenda on Children’s Mental Health” is available on the surgeon general’s Web site at www.surgeongeneral.gov/cmh/childreport.htm. ▪



