2015 Match Finds Big Jump in Students Choosing Psychiatry
Abstract
Neuroscience advances and the increasing perception of psychiatry as integral to the “house of medicine” may be attracting more graduating medical students to the specialty.
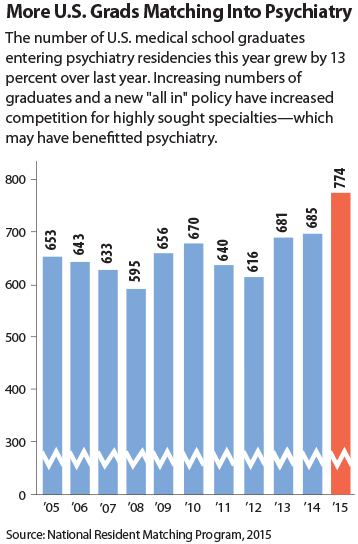
The number of U.S. senior allopathic medical school students entering psychiatry through the National Resident Matching Program (NRMP) increased by 13 percent this year, compared with 2014, with 774 U.S. graduating seniors choosing to enter psychiatry training.

Anita Everett, M.D., chair of the APA Board of Trustees Work Group on Health Care Reform, summarizes the work group’s report at the Board’s meeting last month in Arlington, Va. The work group made a series of recommendations to strategically position APA and American psychiatry to promote and influence U.S. health care reforms.
The outcome for psychiatry in this year’s match is unusually good: the percentage of seniors selecting psychiatry rose from 4.2 percent in 2014 to 4.6 percent in 2015—a larger percentage increase than any other specialty in the match.
The increase of 89 students selecting psychiatry this year compared with last year (see chart on page 10) exceeds that of family medicine, emergency medicine, and general surgery—all of which have many more residency positions than psychiatry. (Only internal medicine—which experienced an increase of 150 students over 2014—had a larger jump in numbers than psychiatry.)
“This is great news,” said Tristan Gorrindo, M.D., APA’s director of education, in comments to Psychiatric News. “In my own experience of working with medical students, I see two potential contributors. First, as we include more neuroscience in medical student education, students see the promise of new and exciting treatments. There is a general sense that we are on the verge of a number of breakthroughs and that the treatments we will have in 10 years will be much more advanced than what we have now. And it’s exciting to be part of this revolution in medicine.
“Additionally, as psychiatry begins to work in closer collaboration with primary care through new models like the patient-centered medical home, I think students like the idea of seeing themselves remaining within the ‘house of medicine,’ ” Gorrindo said. “The ability to be part of a primary care team but to offer specialized expertise on some of the problems that so vex our primary care colleagues allows students to feel as though they are making a valuable contribution to the overall care of patients.
“My hunch is that we’ll see this trend continue with more students going into psychiatry each year,” he said.
The annual match, in which the choices of graduating medical students are paired with those of residency programs seeking trainees, is typically watched as an indicator of workforce size and makeup of the various medical specialties for the coming years.
Sidney Weissman, M.D., a former APA trustee who has long held an interest in workforce issues, said he believes that increasing competition for slots has led many medical students to seek out positions in more than one specialty. “Psychiatry did well in this year’s match, as senior medical students aware of the limited number of residency positions in the most sought-after specialties are considering more options as they plan their medical careers,” he said. “This is why many of us have interviewed applicants matching in more than one specialty. This response from an expanding pool of U.S. graduates is likely to continue into the foreseeable future.”
Weissman noted that in 2018, unless the present cap on Medicare funding for new positions is lifted, U.S. medical schools will graduate 21,000 allopathic and 8,000 osteopathic students. “This number will approximate the number of available PGY-1 positions,” he said. “As the decade progresses, I would predict for these reasons that we will have 1,000 U.S. graduates entering psychiatry, by combining allopathic and osteopathic graduates by 2018.” ■
This year’s match results can be accessed here.



