Study Suggests Neural Correlates Related to Abstinence in Alcoholics
Abstract
After reading an AA prayer, subjects’ reports of craving were lower, and the decrease was correlated with the degree of involvement in AA.
A reduction in the subjective experience of craving among members of Alcoholics Anonymous (AA) with long-term sobriety may reflect the impact on neural mechanisms for management of attention and emotion of their experience in AA and spiritual exercises associated with membership in AA.
Marc Galanter, M.D., says that when people with alcoholism who have been in recovery for a long time are confronted with triggers that had once led to alcohol consumption, areas of the brain associated with attention and control of emotion and with semantic reappraisal of emotional responses are activated.
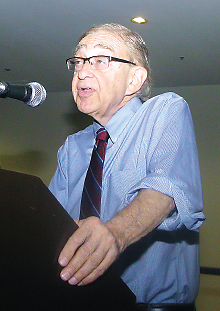
At APA’s 2015 annual meeting in Toronto, psychiatrist Marc Galanter, M.D., director of the Division of Alcoholism and Drug Abuse at New York University School of Medicine, described preliminary research using functional magnetic resonance imaging (fMRI) to demonstrate the neural correlates of diminished alcohol craving in a controlled setting.
When Galanter and colleagues surveyed long-term members of AA, they found that these individuals typically reported little or no craving for alcohol in their daily lives. In an interview with Psychiatric News after the symposium, Galanter pointed out, “These are people who have experienced a lot of craving before they became members of AA and are the people who patients will encounter when psychiatrists suggest they go to an AA meeting.”
Galanter and colleagues employed AA-related prayers as a proxy for the fellowship’s approach to suppression of craving. Photographs related to drinking were shown to subjects while they were in an fMRI scanner after reading neutral material and also after reading AA prayers (such as the “Serenity Prayer”).
The researchers found that subjects’ reports of craving were lower following the AA prayer and that this decrease was correlated with the degree of involvement in AA. Moreover, the prayer effect was found to be associated with the prefrontal and parietal areas of the brain related to attention and control of emotions and with the posterior temporal areas related to semantic reappraisal of emotion.
“In the laboratory we were able to expose these long-term members of AA to pictures of alcohol triggers to see whether they had neural responses and whether there would be a difference in their response depending on whether they recited AA prayers or read neutral material,” Galanter told Psychiatric News. “We thought this would represent the impact of AA on their craving.
“What we found relative to the neutral situation was that [while reading AA prayers] in response to the triggers, these individuals had less response subjectively, and on neural examination there was an alteration in attentional function in the prefrontal cortex and in areas associated with semantic interpretation of stimuli,” he said. “There appears to be a conditioning of certain subjective responses to alcohol triggers that are altered when someone has been in AA for a long time.”
Galanter emphasized that the research is preliminary and needs to be replicated. Nonetheless, he said the findings are significant because they help to clarify why long-term AA members have diminished vulnerability to relapse. “They may also shed light more generally on the nature of successful long-term abstinence in alcohol-dependent people,” he said. “Techniques of modifying a conditioned response to alcohol triggers, as in AA, may represent an option for treating alcohol use disorders.” ■
A video of Galanter discussing his research can be accessed here.



