Saliva Biomarkers May Predict How Long Concussion Symptoms Will Last in Youth
Abstract
Providing a more accurate assessment of patients at greatest risk for prolonged concussion symptoms could help guide treatment plans.
Concussion symptoms tend to resolve in most youth within two weeks, but a third of these patients will continue to experience concussion symptoms for much longer.

Without an accurate, objective measure to determine children most likely to experience prolonged concussion symptoms (PCS), delays in treatment can occur.
A study published online November 20, 2017, in JAMA Pediatrics suggests that measuring the salivary levels of five microRNAs (miRNAs)—small, noncoding RNA molecules that influence protein production throughout the body—can identify children with PCS with greater accuracy than the Sport Concussion Assessment Tool (SCAT3), the tool currently used to determine PCS.
“The miRNAs associated with PCS have potential utility as a toolset for facilitating concussion management,” Steven Hicks, M.D., Ph.D., and colleagues wrote. “This tool could ease parental anxiety about expected symptom duration. An objective PCS tool could also inform clinical recommendations about return-to-play and school-based accommodations.”
The SCAT3 gauges symptom burden based on assessments of the severity of common postconcussive symptoms, including headaches, fatigue, and memory loss. A patient with a high SCAT3 score a few days after experiencing a concussion is thought to be more likely to have PCS. This tool is moderately effective at predicting PCS risk, but it is not objective, because it is based in part on how the patient and parent estimate symptom severity.
To determine the efficacy of salivary miRNAs for determining PCS risk in youth, Hicks, an assistant professor of pediatrics at Penn State College of Medicine, and his team took saliva samples and performed SCAT3 assessments on 52 youth aged 7 to 21 (30 males, 22 females) who had been diagnosed with a mild traumatic brain injury in the past 14 days. The participants were re-evaluated with SCAT3 after four weeks, and patients with symptom scores of 5 or more were designated as having PCS. A total of 30 youth met the criteria for PCS.
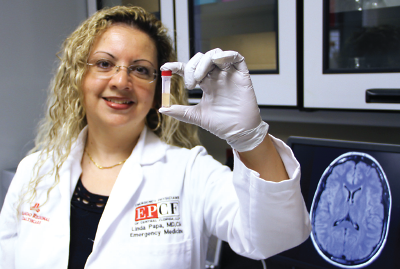
Linda Papa, M.D., believes microRNAs can be useful biomarkers to predict the consequences of a concussion, but cautions that their levels fluctuate following a head injury so the timing of any blood or saliva test is important.
The researchers analyzed over 400 miRNAs from the patient saliva samples and identified 15 miRNAs that were expressed differently among youth with and without PCS. With additional analysis, the researchers narrowed in on a set of five miRNAs (miR-320c-1, miR-133a-5p, miR-769-5p, let-7a-3p, and miR-1307-3p) that proved the most accurate at distinguishing patients with PCS from patients whose symptoms resolved. This panel was able to identify children with PCS with about 85 percent accuracy. In comparison, the SCAT3 was about 65 percent accurate at predicting youth with PCS.
“Now that we have a set of good candidates, physicians can measure these miRNAs easily,” Hicks said. He noted that an miRNA profile can be obtained in about 10 to 15 minutes using a polymerase chain reaction (PCR) machine, which can be found in most hospitals. In addition, saliva can be readily collected in nonclinical settings such as athletic fields, so a sample can be obtained immediately after a head injury occurs, he said.
Linda Papa, M.D., an emergency medicine physician at Orlando Regional Medical Center who has conducted extensive research on concussions, told Psychiatric News that these results are very promising. She has studied miRNAs as biomarkers in adults with traumatic brain injury and found that changes in miRNA expression in the blood shortly after an injury correlate with subsequent clinical outcomes.
“The fact that these biomarkers were obtained from an easily accessible fluid, rather than blood or spinal fluid, is particularly nice as it limits discomfort to children,” Papa said.

One of the advantages of developing saliva-based biomarkers is that saliva samples can easily be taken immediately after a head injury occurs on an athletic field, according to senior study author Stephen Hicks, M.D.
Timing is crucial, however, as these biomarkers can fluctuate dramatically in the hours and days following a concussion, she said. In March 2016, for example, Papa coauthored a study that identified two potential protein biomarkers that could be used to diagnose a concussion up to one week after the fact (Psychiatric News, May 20, 2016). These two proteins became elevated in the blood very quickly following a concussion, but their peak expression and subsequent decline had different trajectories. Thus, the accuracy of the test changed depending on when the blood was drawn.
“A test that’s reliable one day after a concussion may be less so three days later, or vice versa,” she said. Moving ahead, it will be important to track the time course of these miRNAs after an injury and possibly identify the best window to obtain samples.
Hicks and colleagues are conducting an ongoing study in which they are collecting samples at various times after an injury and hope to address the temporal question soon.
Still, Hicks cautioned that “a saliva test is not going to be the sole answer” to diagnosing PCS. “Ideally, it would be part of a broad screening panel that includes other objective measures like eye tracking and EEG (electroencephalography).”
This study was funded by a grant from the Children’s Miracle Network and a research agreement with Quadrant Biosciences; Hicks is a paid consultant for Quadrant. ■
An abstract of “Association of Salivary MicroRNA Changes With Prolonged Concussion Symptoms” can be accessed here.



