Experts Offer Guidance on Medication Management of Acute Agitation
Abstract
Acute agitation can be successfully treated with multiple oral and injectable medications, said experts at the Annual Meeting.
Timely management of acute agitation is important, but knowing the right medication is difficult, as available studies have combined data from patients with a variety of illnesses (for example, patients with schizophrenia, bipolar disorder, substance use disorder), different treatment settings, and different agitation rating scales.
During a session at APA’s 2023 Annual Meeting David N. Osser, M.D., and Sean R. Stetson, M.D., of the Veterans Affairs (VA) Boston Healthcare System discussed their recent efforts at comparing all this disparate data to develop updated guidance on which medications are best for acute agitation due to psychosis or mania.
The first decision involves the route of administration; Osser noted the route is dictated by the level of cooperation from the patient, with oral medication preferred whenever possible.
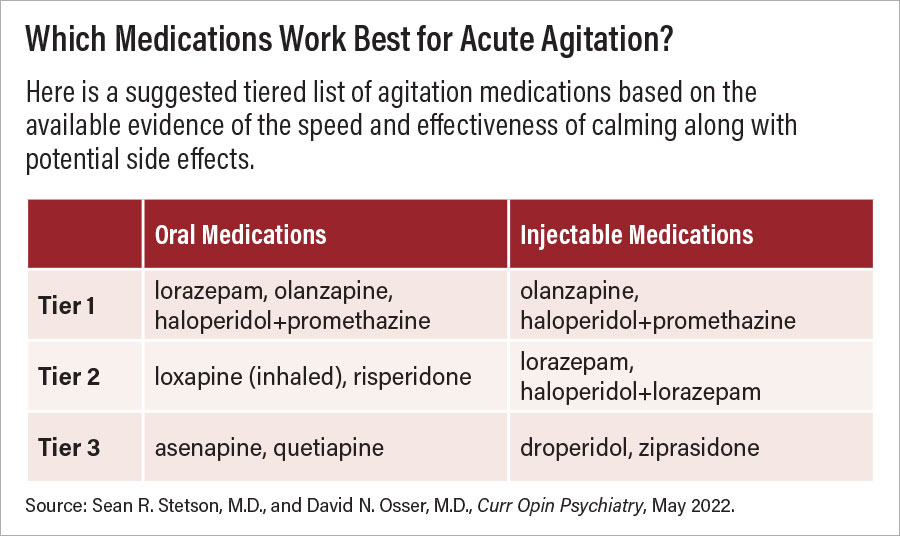
Among oral medications, three are considered “top tier” options: olanzapine, lorazepam, and haloperidol plus lorazepam. “Twenty years ago, haloperidol plus lorazepam was a clear number one, and it still has the long reputation,” Osser said. More recent research has suggested that this combination may not work as quickly as olanzapine and doesn’t offer much more benefit than lorazepam alone. Some second-tier oral options include risperidone and inhaled lozapine.
If a patient requires an intramuscular injection, the top-tier options include olanzapine as well as haloperidol plus promethazine (antihistamine sedative). The latter combination is backed by multiple positive efficacy studies but is not widely used in the United States, Stetson noted. Instead, it is more common for patients in U.S. hospitals to receive a three-drug injectable cocktail that combines haloperidol, lorazepam, and the antihistamine diphenhydramine.
“Interestingly we could find no controlled studies with this cocktail, so we would suggest caution considering there are effective one- and two-drug combinations,” he said. Some second-tier injectable options include haloperidol plus lorazepam or lorazepam alone.
There are other factors to keep in mind when considering medications for acute agitation, the speakers noted. For instance, while midazolam can help to reduce symptoms more rapidly than some of the other medication options, its effects don’t last as long, and repeated dosing may lead to respiratory suppression, Osser noted. In settings where respiratory support devices are available (for instance, emergency department), repeated administration of midazolam may be fine, but he advised against its use in other hospital settings.
Osser also raised concerns about possible side effects associated with dexmedetomidine (Igalmi), which the FDA approved for bipolar or schizophrenia agitation just last year. He noted that the pharmacology newsletter The Medical Letter on Drugs and Therapeutics recently highlighted some potentially concerning side effects of the medication, including orthostatic hypotension.
“Igalmi is not quite ready for a spot in the sequence of medications just yet, but we are keeping our eyes on it,” he said.
Osser and Stetson’s guidance (which includes more details on the tiers as well as dosing recommendations) was published in 2022; Osser plans to add these recommendations to the Harvard South Shore Psychopharmacology Algorithms Project, which offers step-by-step medication guidance for a range of psychiatric conditions. ■



