Psychiatrist Offers Strategies for Treatment-Resistant Depression
David Brent, M.D.: “When family members believe that the teen has control over the symptoms and is simply being manipulative, they don’t support the treatment, which increases the dropout rate.”
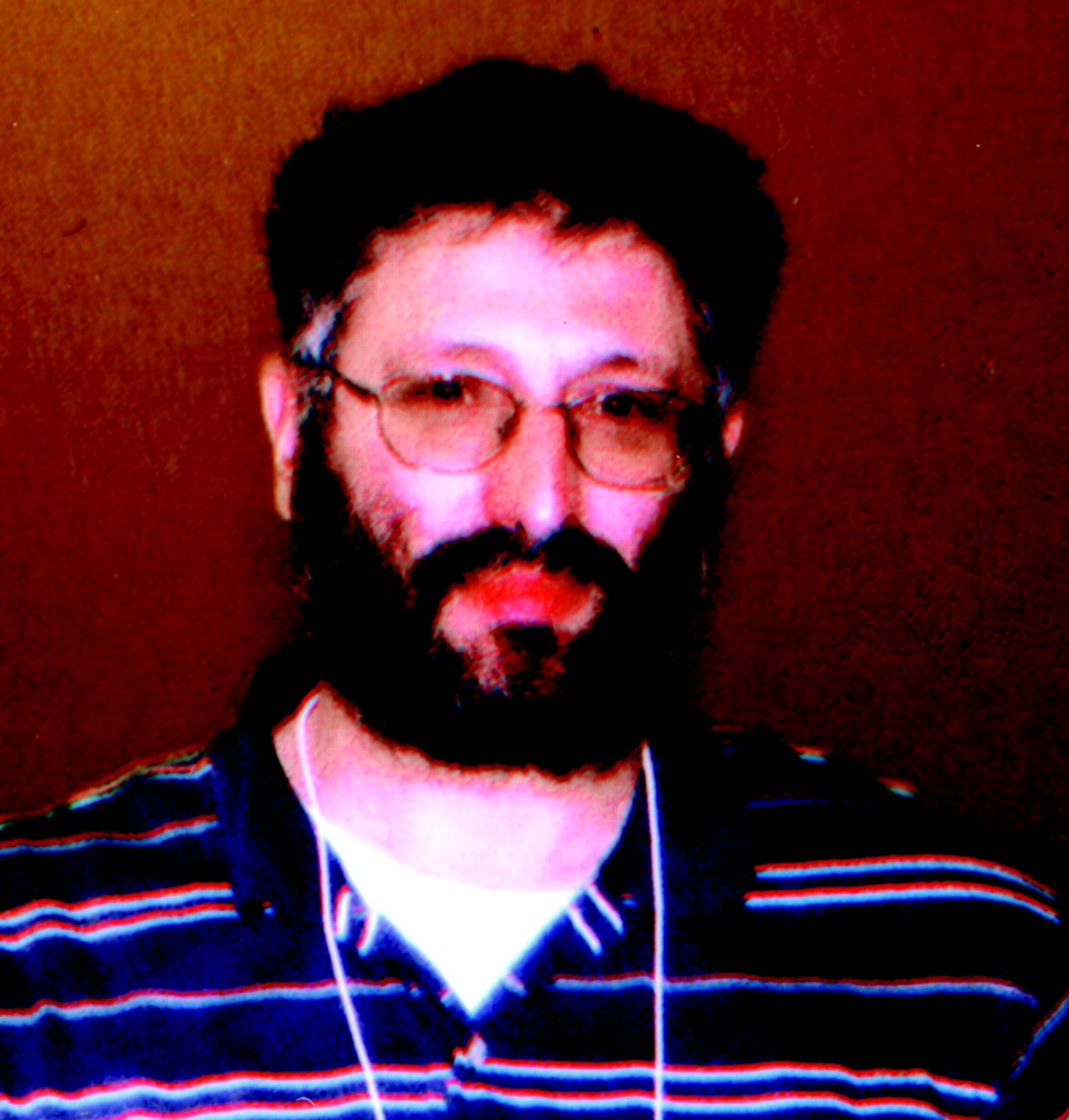
Brent is a child and adolescent psychiatrist who knows all too well the problems associated with treating youth with chronic depression. He directs a clinic for teens with depression and/or suicidality at Western Psychiatric Institute and Clinic in Pittsburgh and has conducted several research trials on depression in adolescents.
“I became interested in treating resistant depression about five years ago when I noticed that more teens were coming to our clinic who hadn’t responded to multiple antidepressants and psychotherapy,” said Brent at the annual meeting of the American Academy of Child and Adolescent Psychiatry in Honolulu in October.
“In contrast to youths with first episodes of depression, who were fairly easy to treat, these youths had recurrent episodes of depression that averaged eight months, substantial comorbidity, and greater initial impairment,” added Brent.
He and his colleagues found several factors besides depression that contribute to treatment resistance. For example, some patients had bipolar disorder, attention-deficit/hyperactivity disorder (ADHD), substance abuse, or a parental history of depression, said Brent. He recommended determining whether these disorders precipitated the depression and then treating the patient for the more serious problem first. There may also be environmental factors at work—including a family history of trauma, abuse, or discord—that may require psychotherapy and medications. A medical illness such as thyroid disease or anemia should also be ruled out, suggested Brent. Early identification and treatment of patients with multiple problems often lead to less treatment resistance, said Brent.
If depression is the primary diagnosis, Brent recommended educating the patient and family members about the illness, treatment, and side effects to enhance compliance.
“I learned from experience that when family members believe that the teen has control over the symptoms and is simply being manipulative, they don’t support the treatment, which increases the dropout rate,” said Brent.
He also recommended talking to the patient and family at the beginning of treatment about the possibility of multiple medication trials, which is common for patients with chronic depression.
An estimated 40 percent of youngsters being treated for depression were found to fail on an initial trial of a selective serotonin reuptake inhibitor (SSRI), which is typically the first treatment for adolescent depression, according to Brent. Similar treatment failure rates were found for psychotherapy including cognitive-behavioral therapy (CBT), he said. However, when CBT or another form of psychotherapy was combined with an antidepressant, the response rate increased to roughly 70 percent, he added.
“Before concluding that an adolescent’s depression is treatment resistant, an adequate dose of an SSRI should be given for at least four weeks and the patient’s response evaluated,” he said. If symptoms appear to improve by 50 percent or more, Brent advised keeping the patient on the same dose. Otherwise, he recommended increasing the dose and observing the patient for another four weeks.
For example, an adequate dose of fluoxetine (Prozac) is 20 mg, and the maximum dose is between 40 mg and 60 mg. These doses are supported by empirical studies in depressed adolescents, said Brent. If one SSRI doesn’t work after eight weeks, the clinician should consider switching to another SSRI on the basis of side effects.
“If a patient is having trouble sleeping, a clinician can try a more sedating SSRI like fluvoxamine [Luvox] or paroxetine [Paxil]. If the patient is fatigued, a more activating agent like fluoxetine may be needed,” said Brent.
If the patient fails on two SSRIs, Brent recommended trying a different class of agents. If the patient has comorbid anxiety and needs to be more alert, then venlafaxine (Effexor) should be considered because it targets both the serotonergic and noradrenergic systems, said Brent. Studies in adults have also found venlafaxine works better than fluoxetine or paroxetine when given at doses of 150 mg or more, he added.
If the patient needs more sedation, then switching to nefazodone (Serzone) or mirtazapine (Remeron) should be considered. If the patient needs to be more alert or has evidence of ADHD or bipolar disorder, bupropion (Wellbutrin) should be considered, said Brent.
If these agents don’t improve the patient’s symptoms by 50 percent or more and the patient has comorbid anxiety, then clomipramine (Anafranil), a tricyclic, may be useful. One study has suggested that intravenous administration may convert nonresponders to responders. But the side effects and toxicity are disadvantages, said Brent.
Monoamine oxidase inhibitors have been shown useful in adults with atypical depression, bipolar depression, and depression comorbid with anxiety, said Brent. “However, the dietary restrictions are a problem for teens. When they hear that they can’t have pepperoni pizza, they don’t want to take it.”
Lastly, Brent recommended adding a second medication if the patient has received some benefit from the first one but still has fairly significant residual symptoms, and previous medications haven’t worked.
“I will add an SSRI to bupropion if the patient has some residual anxiety. Conversely, if the patient is improving somewhat on an SSRI, but has residual fatigue, concentration, and motivational problems, I might add bupropion,” said Brent.
Lithium can be added to an SSRI for nonresponders, but the side effects such as weight gain and acne make compliance difficult. ▪



