Decrease ADHD Symptoms, and Pounds May Follow
Quite a bit of research has linked depression and obesity. Now some researchers have coupled attention-deficit/hyperactivity disorder (ADHD) to obesity as well.
Moreover, they have found that treating ADHD in obese individuals who have it seems to help them lose weight.
“This is an intriguing and potentially important preliminary study,” Michael Devlin, M.D., a Columbia University psychiatrist and eating disorders authority, told Psychiatric News. Its findings suggest that a number of obese people have ADHD and that treating their ADHD can help them lose weight.
The lead investigator was Lance Levy, M.S., a Toronto nutritional scientist who runs a private referral practice for obesity management. Results were published online on February 17 in the International Journal of Obesity.
Levy and his coworkers found that over a quarter of 75 severely obese patients referred to their practice reported having ADHD symptoms as children and as adults. Screening of an additional 190 consecutively referred severely obese patients revealed that over a third had ADHD. Furthermore, most of these patients had tried to lose weight but had failed to do so.
Levy and his colleagues thus suspected that some of the symptoms triggered by ADHD—say, inattention, restlessness, distractibility, impulsivity, and novelty seeking—might have sabotaged the weight-loss efforts of patients who had ADHD. Indeed, other research has shown that the personality trait of novelty seeking is strongly associated with obesity in the general population and with obese individuals' difficulty in losing weight (Psychiatric News, May 18, 2007). So Levy and his coworkers launched a study to see whether ADHD treatment might help obese persons achieve long-term weight loss.
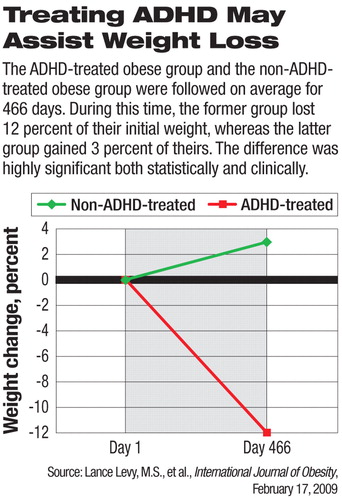
The subjects were 78 severely obese individuals who had been diagnosed for ADHD through clinical interviews. All had tried to lose weight for at least a decade, but had failed. All of the subjects were offered medication treatment for their ADHD. Sixty-five of them accepted medication treatment; the remaining 13 did not. The researchers then followed all of the subjects for at least a year to see whether there was any difference in weight loss between the 65 subjects who were receiving ADHD medication and the 13 subjects who were not. At the end of that period, the group that had received medication had lost 12 percent of their initial weight, whereas the group that had not received medication had gained 3 percent of their initial weight. This difference was highly significant statistically.
“ADHD should be considered a primary cause of weight-loss failure in the obese,” Levy and his coworkers concluded in their study report.“ Screening for ADHD should become part of the diagnostic assessment for the management of severe obesity.”
The study had some weaknesses, Devlin pointed out. For example, it did not include a randomized, control group. It is possible that the psychostimulants used to treat ADHD in 65 of the subjects promoted weight loss not by treating ADHD but by suppressing appetite and increasing energy expenditure.
“It is also important,” he noted, “to recognize that the participant pool consisted of severely obese treatment-refractory individuals seeking further treatment, so the results cannot be generalized to all obese individuals.”
Nonetheless, he said, “that about a third of the severely obese treatment-refractory group were diagnosed with ADHD based on a careful assessment is very thought provoking.... For me, the one thing that this study points to is the utility of carefully identifying and treating both medical and psychiatric comorbid conditions and the degree to which this can improve weight outcomes in those with severe and/or treatment-refractory obesity.”
The study had no outside funding.
An abstract of “Treatment of Refractory Obesity in Severely Obese Adults Following Management of Newly Diagnosed Attention-Deficit/Hyperactivity Disorder” is posted at<www.nature.com/ijo/journal/vaop/ncurrent/abs/ijo20095a.html>.▪



