Torrey Addresses Mistakes Leading to Public MH Crisis
Abstract
E. Fuller Torrey, M.D., says the crisis of homeless people with mental illness on the streets of America stems from a history of well-intentioned but misguided public policies.
American psychiatry and the public mental health system must work to correct policy mistakes that have led to a public health travesty: criminalization of people with mental illness by placing them in jails and prisons and the failure to treat homeless individuals with serious mental illness (SMI).

APA held its fall conference—IPS: The Mental HealthServices Conference—last month in New York. Gathering for a photo before the Opening Session were (from left) APA’s CEO and Medical Director Saul Levin, M.D., M.P.A.; APA President Bruce Schwartz, M.D.; Keynote Speaker E. Fuller Torrey, M.D.; APA President-Elect Jeffrey Geller, M.D., M.P.H.; and Afzal Javed, M.D., president-elect of the World Psychiatric Association (WPA). This year’s IPS was held in collaboration with the WPA.
That’s what E. Fuller Torrey, M.D., said during a keynote address at last month’s Opening Session of APA’s IPS: The Mental Health Services Conference in New York. Torrey is the founder of the Treatment Advocacy C enter (TAC) and associate director for research at the Stanley Medical Research Institute (SMRI). The TAC promotes laws, policies, and practices for the delivery of psychiatric care and supports the development of innovative treatments for severe and persistent psychiatric illnesses and research into their causes. According to the SMRI website, “SMRI has a close relationship with and is the supporting organization for the Treatment Advocacy Center.”
During his address, he detailed a history of tragic public policy blunders: the emptying of state psychiatric hospitals, passage of the Community Mental Health Act (CMHA) with no mandated provisions for care after people with SMI were discharged from state hospitals, and federal financial incentives that encouraged states to abdicate responsibility for this population.
The introduction of Medicaid provided federal funding for people with SMI whose care was previously paid for by the state; this created an incentive for states to close the facilities they funded on their own and move patients into community hospitals and nursing homes partially paid for by Medicaid and the federal government, Torrey explained.
“In summary, we emptied the state hospitals and provided federal fiscal incentives to make sure it happened,” Torrey said. “We began a new program of community mental health centers that was targeted to prevent mental illness but ignored patients discharged from the state hospitals. And we partially federalized what had been a state responsibility with no provisions for the most seriously mentally ill.”
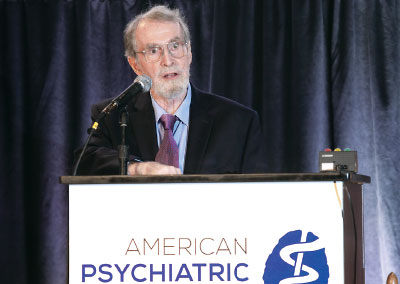
E. Fuller Torrey, M.D., describes how community mental health centers as envisioned by the Community Mental Health Act had no mandate to serve people with serious mental illness.
Torrey, who is also a professor of psychiatry at the Uniformed Services University of the H1 ealth Sciences, has for decades been a fierce advocate for people with serious mental illness in the public sector.
From 1976 to 1985, Torrey was on the clinical staff of St. Elizabeths Hospital in Washington, D.C., where he specialized in the treatment of people with severe psychiatric disorders. From 1988 to 1992, Torrey directed a study of identical twins with schizophrenia and severe bipolar disorder at the National Institute of Mental Health.
Torrey received a Special Presidential Commendation from APA in 2014. He has also received two Commendation Medals from the U.S. Public Health Service, and a Special Families Award from the National Alliance on Mental Illness (NAMI) in 1984.
In a 2007 Psychiatric News profile, past APA Trustee Roger Peele, M.D., said Torrey helped move American psychiatry from a psychoanalytic foundation to a biological one. “His provocative books … contributed to a focus on the biological,” Peele said. “He is combative—when public agency chiefs heard he was due to be on national TV, they ran to their bunkers—and he has used pithy public pronouncements to hammer home the need for public research monies to be devoted to a biological understanding of people with the most disabling of psychiatric illnesses.”
It was Peele who, as chair of the Department of Psychiatry at St. Elizabeths, hired Torrey as a staff psychiatrist in 1977.
In his address last month, Torrey drew attention to a grim irony: The founders of APA 175 years ago were concerned about and discussed the practice of locking up people with mental illness in jails and prisons. These discussions were instigated by Dorothea Dix, who had been outraged by what she saw when she toured the jails and prisons of Massachusetts.
This year, Torrey said, a detention center in Georgia became the first jail to be accredited as a mental health facility by the National Commission on Correctional Health Care. Torrey wondered, “What would Dorothea Dix say of us today?”
He emphasized that the motives that led to deinstitutionalization were good: treatment in the “least restrictive environment” in the community was regarded as an ideal. And he noted that the process of emptying the state hospitals did not begin with the CMHA but with the introduction of chlorpromazine (Thorazine).
However, he said, the vast majority of community mental health centers created by the CMHA—having no mandate to treat discharged patients—operated as private psychiatric clinics focused on prevention rather than treatment. Torrey said IPS is a crucial venue for addressing the problems caused by past errors and looked to young psychiatrists in the audience for solutions.
“Rarely have so many well-meaning people been so wrong,” Torrey said. “My generation made major mistakes in emptying the state hospitals without thinking about how to treat the seriously mentally ill in the community. It is up to the next generation to solve those problems.” ■



