Brain Protein Could Be Treatment Breakthrough
It looks as though a small protein discovered in horses' brains 75 years ago, and since dubbed substance P, may play a role in depression and posttraumatic stress disorder (PTSD).
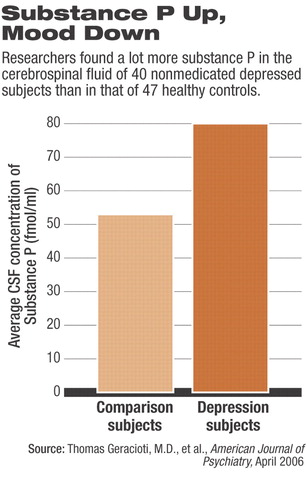
Thomas Geracioti, M.D., a professor of psychiatry at the University of Cincinnati, and his colleagues compared the levels of substance P in cerebrospinal fluid taken from 40 nonmedicated subjects with major depression with that from 47 healthy comparison subjects.
The levels of substance P from the depressed subjects, they found, were much higher than those from the controls (see chart).
The researchers then measured the levels of substance P in cerebrospinal fluid taken from eight nonmedicated subjects with PTSD and from eight healthy matched subjects. The levels of the PTSD subjects were significantly higher than those of the controls.
“These results suggest that elevated central nervous system substance P concentrations are involved in both major depression and PTSD,” Geracioti and his group concluded in their report in the April American Journal of Psychiatry.
Moreover, the researchers exposed seven combat veterans with chronic PTSD and not on any medications to two stimuli. One was footage from the Vietnam War, which was presumably upsetting to the subjects; the other was a film instructing viewers how to oil paint, which presumably did not arouse the subjects emotionally.
The investigators measured the subjects' cerebrospinal levels of substance P during each of the two viewings and then compared the levels.
When the subjects viewed the war footage, their levels of substance P shot up, which was not the case when they looked at the painting-instruction film. So substance P responds dramatically to psychological stress in PTSD subjects, and this response may be one of the mechanisms by which psychological trauma unleashes PTSD symptoms, the researchers suggested.
Finally, the study results suggest that if substance P is complicit in depression and PTSD, then chemical compounds that counter substance P might be able to attenuate these two mental illnesses.
Indeed, Geracioti told Psychiatric News, many drug companies are developing substance P antagonists, and a few—notably GlaxoSmithKline, Hoffmann-LaRoche, Merck, and Pfizer—are testing some of these antagonists in depressed subjects to see whether the antagonists might improve their depression.
Furthermore, Geracioti said, psychiatrist Dennis Charney, M.D., of Mount Sinai School of Medicine, recently launched a trial funded by the National Institute of Mental Health to see whether a particular substance P antagonist might help subjects with PTSD.
He and his group, Geracioti added, will also be testing a substance P antagonist in PTSD subjects once they reach an agreement with the drug company that makes it.
“Since available treatments for PTSD are typically of limited efficacy,” Geracioti explained, “I have high hopes for the use of substance P antagonists in the treatment of the illness.”
As a matter of fact, Geracioti pointed out, one substance P antagonist is already on the market. It is made by Merck, with the generic name aprepitant and the brand name Emend. It is approved by the Food and Drug Administration for use against chemotherapy-induced nausea and vomiting, in combination with other antiemetics.
“It is intriguing,” said Geracioti, “that patients with PTSD sometimes describe having experienced nausea, or even frank vomiting, as part of a traumatic exposure.”
So could aprepitant help PTSD patients? Maybe. But as Geracioti clarified, even when it is used as indicated it is supposed to be used only for three days and “is very expensive.”
The study was funded by the VA Merit Review and Research Advisory Group, National Alliance for Research on Schizophrenia and Depression, National Institute of Mental Health, and Merck.
“Elevated Cerebrospinal Fluid Substance P Concentrations in Posttraumatic Stress Disorder and Major Depression” is posted at<http:ajp.psychiatryonline.org> under the April issue. ▪



